Living with a long-term lung condition can feel overwhelming at times – but understanding what’s happening in your body is one of the most powerful steps you can take to feel more in control. Whether you’ve been told you have asthma, chronic obstructive pulmonary disease (COPD), or a mix of the two, this article will help you understand your condition and why good management really matters.
🌬️ What’s the difference between asthma and COPD?
Asthma and COPD both affect the airways in your lungs, but they are different conditions – and knowing which one you have (or if you have both) helps you get the right support.
| Feature | Asthma | COPD |
| Cause | Often starts in childhood or early adulthood. May be linked to allergies or triggers like pollution, cold air, or exercise. | Usually develops after age 40. Strongly linked to smoking or long-term exposure to dust, fumes, or chemicals. |
| Symptoms | Come and go. Cough, wheeze, chest tightness, breathlessness, especially at night or early morning. | Ongoing breathlessness, persistent cough with phlegm, and frequent chest infections. |
| Airway narrowing | Usually reversible (with inhalers). | Often irreversible – airways stay narrowed over time. |
| Lung function tests | Typically show variability or improvement with medication. | Usually show permanent changes. |
Some people have features of both asthma and COPD. This is known as Asthma-COPD Overlap (ACO). Your GP or nurse may still call it asthma or COPD depending on which is more dominant, but recognising the overlap helps guide better treatment.
🔥 What’s going on inside the lungs?
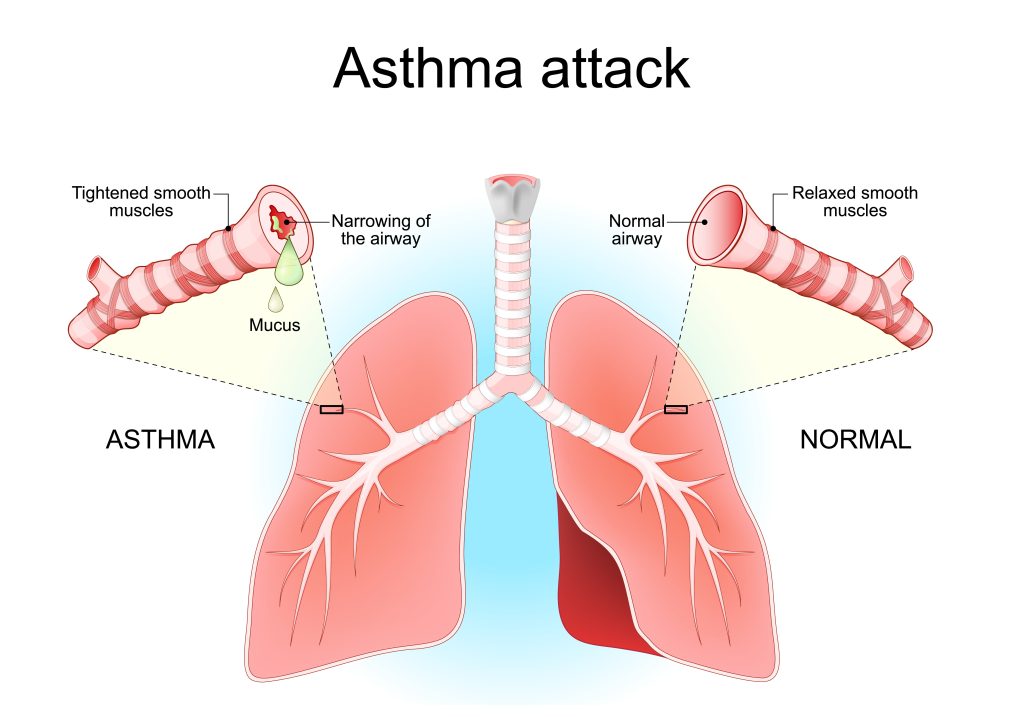
Both asthma and COPD cause inflammation – a kind of swelling and irritation in the airways.
Imagine your airways as a set of tubes. In both conditions:
- The lining of the tubes gets inflamed, making them swollen and sensitive.
- Mucus builds up, making it harder for air to flow.
- The muscles around the airways can tighten, especially in asthma, making breathing feel harder.
In COPD, the tiny air sacs (alveoli) in the lungs can also be damaged. This makes it harder to exchange oxygen and carbon dioxide, leading to persistent breathlessness.
What causes asthma, COPD, and overlap – and why they can flare up
Understanding the root causes and processes behind asthma and COPD can help you take more confident steps to manage them and reduce the risk of flare-ups (exacerbations).
Asthma: A sensitive and inflamed airway
Asthma is a long-term condition where your airways are overly sensitive and prone to inflammation. When triggered, the muscles around your airways tighten, the lining becomes swollen, and mucus is produced – making it harder to breathe.
What causes asthma?
Asthma often develops in childhood or early adulthood, and is influenced by a mix of:
- Genetics: Asthma often runs in families
- Environmental exposures: Dust mites, pet dander, mould, or pollution
- Allergies: Hay fever, eczema, and food allergies are linked to asthma
- Viruses: Respiratory infections early in life may increase risk
- Occupational triggers: e.g. dusts, fumes, or chemicals at work
Some people have allergic asthma, while others have non-allergic asthma triggered more by irritants, cold air, or exercise.
What makes asthma worse?
- Poor medication adherence
- Ongoing exposure to allergens or irritants
- Smoking or second-hand smoke
- Viral infections (like colds or flu)
- Emotional stress or intense exercise without preparation
Knowing your personal triggers is key to preventing and managing flare ups. Keeping a symptom diary can help you identify these triggers and plan accordingly.
COPD: Damage and narrowing over time
COPD (Chronic Obstructive Pulmonary Disease) is a progressive condition that develops slowly over many years, most often due to long-term exposure to harmful particles like tobacco smoke, but also from other inhaled toxins like dust, fumes, or pollution.
It includes:
- Chronic bronchitis: Long-term cough and mucus production
- Emphysema: Damage to the air sacs (alveoli) in the lungs, reducing oxygen exchange
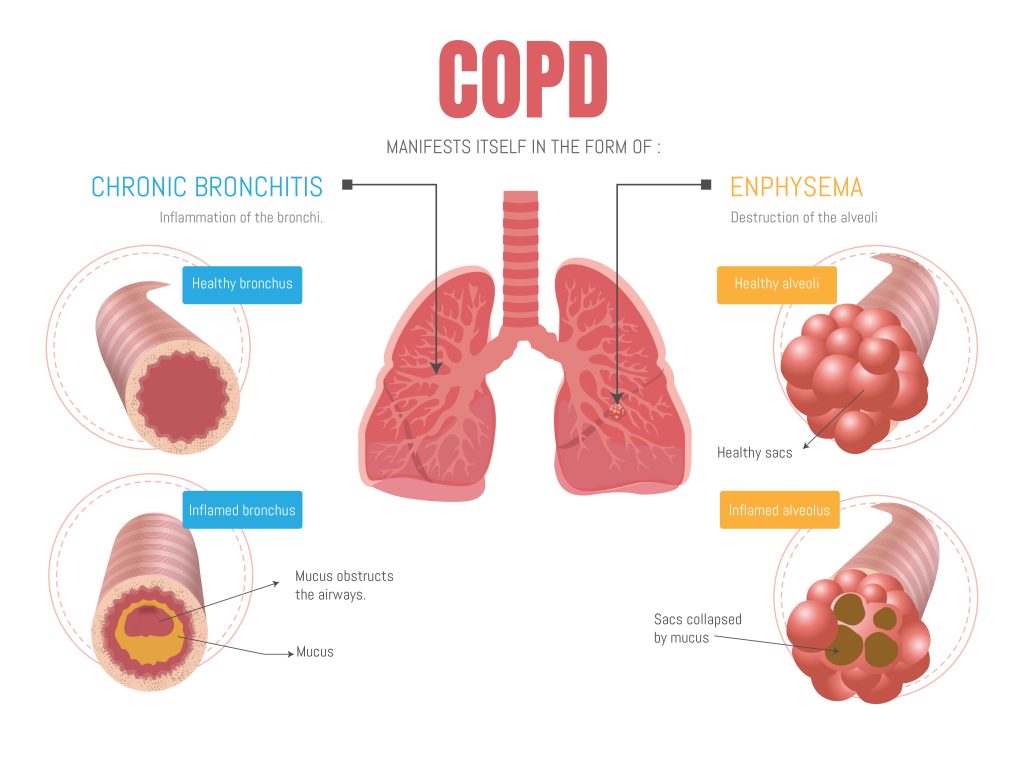
The damage causes chronic inflammation, thickening of the airway walls, mucus buildup, and destruction of lung tissue – all leading to narrowed airways and breathlessness.
What causes COPD?
- Smoking (the main cause in >80% of cases in the UK)
- Occupational exposure: Chemicals, dusts, fumes
- Indoor air pollution: From cooking fuels (more common in low-income countries)
- Genetic conditions like alpha-1 antitrypsin deficiency (rare)
What triggers COPD flare-ups?
- Chest infections (bacterial or viral)
- Changes in weather, especially cold air
- Pollution or strong fumes
- Poor medication adherence
- Dehydration, stress, or other medical illnesses
Flare-ups (also called exacerbations) often require antibiotics, steroids, or hospital treatment and can speed up lung decline if not managed well.
Asthma-COPD overlap: A complex mix
Some people have features of both asthma and COPD, often called Asthma-COPD Overlap (ACO). This is more likely in:
- People with a history of asthma who smoke
- Older adults with both reversible (asthma-like) and fixed (COPD-like) changes in the lungs
Their airways might be swollen and sensitive (chronic inflammation), and the shape of the airways can change over time (remodelling) and thus more reactive to triggers (hyper-responsiveness), making diagnosis and treatment more complex. Treatment usually combines inhaled corticosteroids (ICS) and long-acting bronchodilators (LABA, LAMA) to reduce symptoms and flare-up risk.
You can read more about the different treatments and how they support different aspects of prevention and symptom relief in our article on respiratory medications.
Why does understanding my condition matter?
Understanding the underlying processes helps you see why:
- Regular preventer medication matters (even when you feel okay)
- Trigger avoidance and lifestyle changes help reduce inflammation
- Early treatment of infections or symptoms can prevent serious flare-ups
- Stopping smoking is one of the most powerful ways to slow or even halt COPD progression
With the right approach, many people with asthma or COPD can live full, active lives – with fewer symptoms and better long-term lung health.
Why medication management matters
It can be tempting to only use your medication when you feel unwell—but daily management helps keep your lungs healthier in the long run.
Uncontrolled asthma or COPD can lead to:
- More frequent flare-ups (exacerbations)
- Emergency hospital visits
- Long-term damage to your lungs
- Increased risk of infections
- More impact on your day-to-day life
Good management reduces these risks. By learning to do the following, you take control of your condition instead of letting it control you – and it may even save your life:
- Use your medication correctly and consistently
- Avoid triggers
- Notice changes early
- Take action when needed
- Consult healthcare professional to prevent further attacks
- Adjust medication and personal action plan if needed
This approach, known as supported self-management, is recommended by national guidelines because it improves wellbeing and reduces emergency care use.
Many people get used to asthma symptoms and don’t realise they could feel better
It’s common for people with asthma or COPD to put up with symptoms like coughing, breathlessness, or waking at night. Over time, they may start to think these symptoms are normal—even when they’re not.
Many people with asthma think their condition is well controlled, even when they have frequent symptoms. In the REALISE survey (REcognise Asthma and LInk to Symptoms and Experience), which included over 8,000 people aged 18–50 from across Europe, more than 80% believed their asthma was controlled, yet nearly half had experienced serious flare-ups in the previous year. Many, especially younger adults, accepted daily breathlessness or frequent reliever inhaler use as normal.
But getting used to symptoms can be risky. It can mean:
– Not asking for help, even though treatment could help a lot
– A higher chance of flare-ups or asthma attacks
– Patients and doctors thinking things are fine when they’re not
Good control means feeling well most days, with little or no need for a quick-relief inhaler. If you’re having regular symptoms, it’s worth speaking to your GP or asthma nurse – there may be better options for managing your condition.
💪 Why healthy habits make a real difference
Living with a respiratory condition doesn’t mean you can’t feel well, strong, and in control. In fact, developing simple, sustainable lifestyle habits can play a powerful role in reducing your symptoms, slowing down disease progression, and improving your energy and quality of life.
The NHS and leading respiratory guidelines encourage a whole-person approach, not just medication. That’s because your lungs don’t work in isolation – they’re part of a system that thrives when you take care of your body and mind.
Here are the six key pillars of lifestyle medicine that can support your lung health:
🥦 1. Healthy eating
Eating a balanced, mostly whole-food diet can reduce inflammation, support immunity, and help maintain a healthy weight – which makes breathing easier.
Diets rich in fruit, vegetables, fibre, and healthy fats (like olive oil and nuts) have been shown to support lung function and reduce flare-ups.
Here’s our article on what makes up a healthy diet to help you with tips on eating well.
🚶♂️ 2. Physical activity
Moving your body – at your own pace – helps improve lung efficiency, muscle strength, and energy levels. Regular activity also reduces breathlessness over time and improves mood.
Pulmonary rehabilitation programmes are based on this principle and are recommended by NICE and BTS/SIGN guidelines.
Exercise-induced asthma: Staying active, breathing easier
If physical activity brings on coughing, wheezing, or chest tightness, you might have exercise-induced asthma – a common pattern where cold air, dry air, or increased breathing during exercise narrows the airways.
The good news? With the right preparation, most people can exercise safely and confidently. Using a reliever inhaler (like salbutamol) 10–15 minutes before activity can prevent symptoms, and some people benefit from a warm-up routine and wearing a scarf over the mouth in cold weather.
If symptoms still break through, you may need a daily preventer inhaler or combination treatment – speak to your nurse or doctor. Regular movement is good for your lungs, heart, and mental wellbeing – and asthma should never stop you from staying active with the right support.
🧘♀️ 3. Managing stress
Stress and anxiety can make breathlessness feel worse. Calming your nervous system with simple breathing exercises, mindfulness, or talking therapies can reduce this vicious cycle. It’s about feeling safe in your body again.
Managing fear during an asthma or COPD attack
It’s natural to feel panicked during an asthma flare-up or COPD exacerbation – shortness of breath and tightness can trigger intense fear – and that fear often makes breathing even harder.
Research shows that learning simple breathing techniques like slow diaphragmatic breathing and pursed-lip breathing can reduce anxiety, calm your nervous system, and help you regain breath control.
Techniques taught in Cognitive Behavioural Therapy (CBT) – such as recognising unhelpful thoughts, using relaxation strategies, and gradually confronting breathlessness – can prevent panic attacking your symptoms and improve your confidence with breathing.
In people with COPD, these approaches have been shown to limit activity avoidance, lift mood, and reduce flare-ups of breathlessness-linked anxiety (https://pubmed.ncbi.nlm.nih.gov/23882107/, https://pubmed.ncbi.nlm.nih.gov/32808571/, https://pubmed.ncbi.nlm.nih.gov/39477355/).
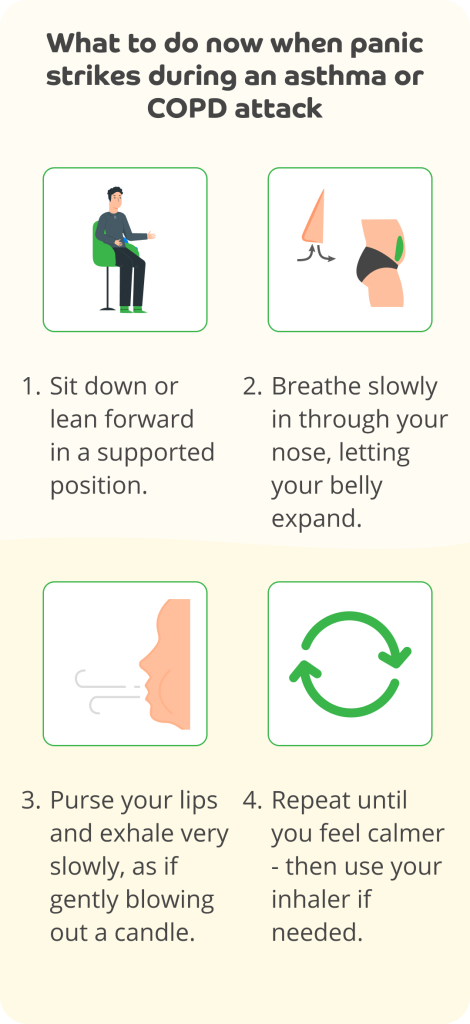
Practising these steps regularly outside of attacks (e.g., daily), reduces fear in future episodes and gives you a tool to regain composure when breathlessness hits.
😴 4. Sleep
Good-quality sleep helps your body repair and supports your immune system. Poor sleep can increase inflammation and worsen fatigue, making symptoms harder to manage. Addressing sleep issues (like waking at night with symptoms) is an important part of asthma and COPD reviews. Our 15 tips for better sleep may help.
🚭 5. Avoiding harmful substances
The single most important lifestyle step for COPD (and for some with asthma) is stopping smoking. Quitting smoking can slow or even halt progression of COPD and improve day-to-day breathing. It’s never too late to stop – and you don’t have to do it alone. NHS stop smoking services really work. Take a look at our article on how to quit smoking here.
👥 6. Connection & support
Feeling supported by others – whether through family, peer groups, or professionals – can boost your ability to make positive changes and stay well. You’re more likely to stick with new habits when you don’t feel alone.
Here are some examples of organisations that run support groups:
- Asthma + Lung UK Breathe Easy Groups
Website: Asthma + Lung UK Support Groups: https://www.asthmaandlung.org.uk/support-you/breathe-easy-support-groups
Asthma + Lung UK run over 150 local ‘Breathe Easy’ groups across the UK. These are peer-led support groups where people with asthma, COPD and other lung conditions can:
- Share experiences and tips
- Learn from expert guest speakers (e.g. nurses, physios)
- Take part in gentle exercise, singing for lung health, and more
- Access emotional support and education
You can search by postcode on their website to find your nearest group or join online sessions.
- BLF Online Community (Now part of Asthma + Lung UK)
Website: HealthUnlocked Lung Health Forum (https://healthunlocked.com/blf) This online community hosted by HealthUnlocked allows people with asthma, COPD, and other lung conditions to:
- Post questions and share experiences
- Get support anonymously
- Access moderation from trained patient champions and charities
- NHS Pulmonary Rehabilitation Programmes
Many local NHS pulmonary rehab services include or link with peer support networks, especially for COPD. You can:
- Ask your GP or respiratory nurse about referral to a local PR programme
- Check local NHS Trust websites or respiratory service hubs
- In some areas, peer groups continue after rehab ends
- Facebook groups and local charities
While not all are professionally moderated, many local Facebook groups or community centres host lung health meetups. Search terms like:
- “Asthma support [your town]”
- “COPD group [your area]”
- “Breathe Easy [county]”
Some examples include groups run by Age UK, respiratory health charities, and community wellness hubs.
🧠 Change is easier when it feels meaningful, manageable, and supported. We’ll help you build habits that fit into your real life – not someone else’s ideal.
🛠️ Takeaway actions
✔️ Learn what type of condition you have and ask your GP or nurse if you’re unsure
✔️ Get to know your triggers and keep track of symptoms
✔️ Don’t wait for symptoms to get worse – your preventer inhalers are key
✔️ Use your action plan to guide you on what to do and when
✔️ Book your annual review and check your inhaler technique
You’re not alone – and you’re not powerless. Understanding your condition is the first step towards managing it confidently and improving your quality of life.
This article is intended for general educational purposes only and does not constitute medical advice, diagnosis, or treatment. It is designed to help adults understand the basics of asthma, COPD, and asthma–COPD overlap syndrome (ACOS), and to empower people to take informed steps toward better self-management in partnership with a qualified healthcare professional.
Do not use this article to diagnose yourself or others, or to make decisions about starting, stopping, or changing any treatment.
If you are experiencing severe breathlessness, chest pain, confusion, or blue lips/fingertips, call 999 immediately.
✅ If you haven’t already, download the free Evergreen Life app to track your health, including managing your asthma and/or COPD, and get practical tips that help you take control of your overall health.





