Breathing is something we often take for granted – until it becomes difficult. If you live with asthma, COPD, or a mix of both, certain breathing exercises may help you feel more in control, reduce symptoms, and improve your quality of life.
This article explains which breathing techniques are backed by good evidence, how they work, and how to try them safely.
🧘♀️ Can breathing exercises really help with asthma and COPD?
Yes, some breathing techniques can:
- Ease breathlessness and chest tightness
- Improve your breathing pattern
- Help you stay calmer during flare-ups
- Support better sleep and physical activity
These exercises won’t replace your medication, but they can be a powerful add-on to your usual treatment. They’re recommended by expert groups like the British Thoracic Society, NICE, SIGN, and GOLD for many people with long-term lung conditions.
🫁 Buteyko breathing
The Buteyko method teaches you slower, gentler breathing through the nose, reducing over-breathing (also known as hyperventilation). and. reducing chest tightness. It may also improve your sense of control over your symptoms.
- Studies show Buteyko can ease breathlessness, improve asthma control and quality of life, and may reduce bronchodilator use (Pfab et al., 2013; Venkatesan et al., 2012; Udayani et al., 2019).
- It may help by reducing hyperventilation and stabilising CO₂ levels, which can relax the airways (Hassan, 2022; Mohamed et al., 2019).
- Early work in COPD suggests Buteyko breathing may support better breathing patterns, ease shortness of breath and improve overall quality of life (Arora et al., 2022, Baig et al., 2024)
- We still need more high-quality trials, but the early signs are promising.
Try it (simple start): Sit tall, close your mouth, breathe gently through your nose, and pause briefly after each soft exhale. Keep shoulders relaxed. Stop if you feel dizzy. If you are not sure, try it with a trained physiotherapist or find a certified Buteyko instructor. Some NHS respiratory clinics offer it.
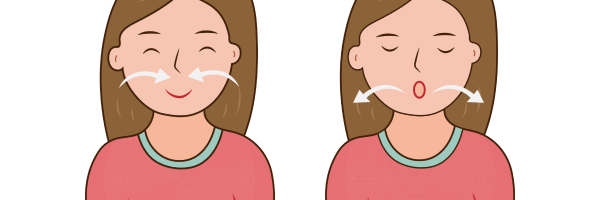
🌬️ Pursed-lip breathing
Pursed-lip breathing is a simple technique used to slow down your breathing and make it easier to empty your lungs. You breathe in through your nose and out slowly through pursed lips (like blowing through a strawier blowing out candle).
- PLB can lower breathlessness, slow breathing, improve oxygen levels, and boost walking distance, especially in COPD (Mulyadi et al., 2022; Parkavi et al., 2022; Budiono et al., 2017; Dhengare & Pohekar, 2021).
- It can also help people with asthma feel less short of breath and breathe more efficiently (Rahmi et al., 2023; Hariyono et al., 2017).
- PLB works by keeping airways open a little longer during the out-breath, which can ease air trapping (Sankar et al., 2020).
- Whilst PLB can be used situations to help ease immediate respiratory distress in can also help day to day, enhancing daily living activities and boosting your confidence in managing your symptoms (Roberts et al.2017).
Try it: Inhale through your nose for about 2 seconds → purse your lips → exhale gently for about 4 seconds. Repeat for 1-2 minutes.
🫀 Diaphragmatic (Belly) Breathing
This technique helps train your diaphragm – the main muscle used for breathing – to work more efficiently. You breathe slowly and deeply into your belly, rather than shallowly into your chest.
This focuses on breathing with the diaphragm rather than the upper chest.
- In COPD it can increase the amount of air moved each breath, slow the breathing rate, and ease breathlessness (Morrow et al., 2016; Prakash et al., 2021).
- It works well when combined with with Pursed-lip breathing and as part of structured professional led pulmonary rehab programmes, improving function and quality of life (Dhengare & Pohekar, 2021; Mendes et al., 2019; Chen et al., 2022).
Try it: One hand on your chest, one on your belly. Breathe in through your nose so your belly hand rises more than your chest hand. Breathe out slowly (pursed lips if helpful).
Slow paced breathing
When we’re anxious, we tend to breathe fast and shallow. This can make breathlessness worse. Slow, steady breathing can help calm the nervous system, reducing that “panic-breathlessness” cycle.
- Slow breathing can reduce over-activity of the stress system and improve symptoms in COPD (Karunarathne et al., 2023).
- In asthma, slow belly breathing with biofeedback (using sensors or simple devices to show you how your body is working, like breathing rate, heart rate, or muscle activity, so you can learn to control it) improved symptoms and quality of life (Ritz et al., 2014).
- Around six breaths per minute may help the body’s natural control systems (including the baroreflex and autonomic stress responses) stay balanced, making it easier to keep blood pressure steady and to cope better when oxygen levels drop. (Critchley et al., 2015).
- Calmer breathing can also lower anxiety, which often worsens asthma and COPD (Greenwell et al., 2021; Bruton et al., 2018; Dhengare & Pohekar, 2021; Sartika et al., 2022).
Try it: One hand on your chest, one on your belly. Breathe in through your nose so your belly hand rises more than your chest hand. Breathe out slowly (pursed lips if helpful).
Active Cycle of Breathing Technique (ACBT)
The Active Cycle of Breathing Technique (ACBT) is a simple set of breathing exercises designed to help clear mucus (sputum) from the lungs. It can make breathing easier, reduce the risk of chest infections, and support better lung function in people with asthma and COPD.
ACBT uses three easy breathing steps, repeated in a cycle, to help clear mucus:
- Gentle breathing – relaxed breaths to calm your lungs and keep your airways from tightening.
- Deeper breaths – slow, fuller breaths (sometimes with a short pause) to get air behind the mucus and help loosen it.
- Huffing – a strong breath out through an open mouth, like steaming up a mirror, to move mucus up where it’s easier to cough out.
By cycling through these steps, you can clear your chest more effectively while keeping your breathing under control.
Research shows that ACBT can:
- Improve lung ventilation and clear secretions more effectively than traditional chest physiotherapy (Pathan et al., 2021; Qureshi et al., 2024).
- Reduce mucus build-up, breathlessness, and the risk of infections, which is especially important in COPD (Baig et al., 2024; Hussain et al., 2022).
- Improve comfort and breathing rates compared with some other airway clearance techniques (Sawitri et al., 2024).
- Help during flare-ups and is widely recommended by physiotherapists for acute and long-term respiratory care (Phillips et al., 2021).
Guideline Support
- NICE (COPD guidelines) recommend chest physiotherapy, including techniques like ACBT, for people with ongoing mucus production and difficulty clearing secretions.
- British Thoracic Society (BTS) physiotherapy guidelines support the use of ACBT as a first-line airway clearance method.
- GOLD COPD strategy highlights airway clearance techniques such as ACBT as part of symptom management in people with significant sputum.
- Joint BTS/SIGN/NICE asthma guidelines note that physiotherapy and breathing techniques may help with mucus clearance in selected patients.
The Takeaway
ACBT is safe, flexible, and can be practised at home once taught by a physiotherapist. For people with asthma or COPD who struggle with mucus, it can improve breathing, reduce infections, and support everyday lung health. You can read more on how to in this guide by Chartered Association of Physiotherapists.
🎵 Singing for lung health
Singing uses controlled breathing and strengthens breathing muscles. It can also lift mood and reduce isolation.
- Singing training can build respiratory support and control (Salomoni et al., 2016; Lewis et al., 2021).
- People with COPD in singing groups report better well-being, less dynamic hyperinflation, and social benefits (Lord et al., 2010; McNaughton et al., 2016; Clark & Harding, 2012).
- Programmes like “Singing for Lung Health” have shown improvements in breathing patterns and quality of life (Lewis et al., 2018; Kaasgaard et al., 2022; Huang et al., 2021).
- British Lung Foundation run “Singing for Lung Health” groups and are available in many areas around the UK.
Guidelines don’t yet single out singing, but they do highlight the wider benefits of pulmonary rehabilitation.
- NICE, GOLD, and BTS recognise that rehabilitation should include psychosocial support. Singing can be seen as part of this – helping with breath control, confidence, and mood, alongside medical care.
Look for local or online lung health singing groups, or try gentle warm-ups, easy scales, and short songs with relaxed, longer out-breaths. Stop if you feel light-headed.
🚶♂️ Pulmonary Rehabilitation Breathing Training (for COPD)
Pulmonary rehabilitation brings many of these breathing techniques and lifestyle approaches together, combining exercise, education and breathing techniques with structured support and guidance from trained professionals to help people manage their asthma or COPD more effectively. The programmes are provided by various different healthcare professionals, including physiotherapists, nurse specialists and dieticians.
- It helps people with COPD by improving exercise capacity, easing breathlessness, lifting mood, and enhancing overall quality of life. Pulmonary rehabilitation also gives individuals a greater sense of control over their condition, and can be delivered through home-based or tele-rehab programmes as well as during recovery from flare-ups. (Zhang et al., 2022; Charikiopoulou et al., 2019; Pierobon et al., 2017; Rahmad et al., 2020; 2015 Cochrane review).
- It can also help reduce hospital admissions and breathlessness in COPD (NICE NG115).
This is one of the strongest recommendations across all the guidelines.
- NICE, GOLD, SIGN, and BTS all advise offering pulmonary rehabilitation to people with COPD who are limited by breathlessness, including soon after an exacerbation.
- PR has also been shown to benefit some people with asthma who have ongoing symptoms or reduced exercise capacity.
- Home-based and online (tele-PR) programmes are supported when centre-based options aren’t possible.
Pulmonary rehabilitation programmes usually involve 2 or more group sessions a week for at least 6 weeks.
A typical programme includes:
- physical exercise training tailored to your needs and ability – such as walking, cycling and strength exercises
- education about your condition for you and your family
- dietary advice
- psychological and emotional support
Ask your GP or nurse if you are eligible for referral to an NHS pulmonary rehabilitation programme if you haven’t attended a programme before and/or read more about them here.
Summary: Breathing techniques you can try
| Technique | May help with | How to start |
|---|---|---|
| Buteyko Breathing | – Feeling less breathless – Reducing need for reliever inhaler – Calming over-breathing | Sit comfortably, close your mouth, and breathe gently through your nose. After each soft exhale, pause briefly before the next inhale. Keep shoulders relaxed. Stop if dizzy. |
| Pursed-lip (PLB) Breathing | – Lowering breathlessness – Slowing breathing rateImproving oxygen levels | Inhale gently through your nose (about 2 seconds). Purse your lips (like blowing out a candle) and exhale slowly (about 4 seconds). Repeat for 1–2 minutes. |
| Diaphragmatic (“Belly”) Breathing | – Improving lung efficiency – Reducing hyperventilationEasing anxiety and tension | Place one hand on your chest, one on your belly. Inhale through your nose so the belly hand rises more than the chest hand. Exhale slowly (through pursed lips if helpful). |
| Slow Paced breathing | – Calming panic-breathlessness cycle – Reducing anxiety and stressImproving overall breathing control | Breathe in gently for 4–5 seconds, then out for 5–6 seconds. Aim for about 6 breaths per minute. Try for 3–5 minutes. |
| Active Cycle of Breathing Technique (ACBT) | – Clearing mucus and easing chest congestion – Preventing infections – Reducing breathlessness linked to sputum | Learn from a physiotherapist: start with relaxed breathing → take a few deeper breaths → finish with “huffing” (a strong breath out, like steaming a mirror) to move mucus up and out. |
| Singing | – Strengthening breathing muscles – Improving mood and social connection – Helping clear mucus | Try gentle warm-ups, easy scales, or short songs. Focus on steady in-breaths and longer, relaxed out-breaths. Join a local “Singing for Lung Health” group if available. |
| Pulmonary rehab | – Improving fitness and exercise capacity – Reducing breathlessness and anxiety – Enhancing quality of life | Ask your healthcare provider about referral to a PR programme. Includes exercise, breathing training, and structured professional support in a group or home-based setting. |
Breathing techniques: What to the guidelines say
The guidelines support breathing retraining, but only as an adjunct (an add-onto other therapies like inhalers):
- BTS/SIGN asthma guidance notes that breathing techniques can help improve quality of life and reduce symptoms, but they should not replace inhaled anti-inflammatory treatments.
- NICE and GOLD highlight the importance of teaching these techniques through physiotherapists or pulmonary rehabilitation programmes so patients get the most benefit.
- Breathing retraining may be especially helpful for people with dysfunctional breathing, anxiety-related breathlessness, or during recovery after exercise.
🗣️ Final thought
Breathing exercises are free, low-risk, and can be done almost anywhere. They won’t cure your condition, but they can help you manage symptoms, reduce anxiety, and feel more in control of your breathing.
Try searching for local “breath easy” or “singing for lung health” groups here.
Consider asking your GP or respiratory nurse specialist to signpost you to local support groups or find out if you are eligible for referral to a pulmonary rehabilitation program.
Start small, be consistent, and talk to your healthcare team about techniques that could work best for you.
If you haven’t already, download the free Evergreen Life app to track your health, including managing your asthma and/or COPD, and get practical tips that help you take control of your overall health.
This article is for education and self-management support only. It does not replace medical advice, diagnosis, or treatment from a qualified healthcare professional.
– Always continue to take your prescribed medicines (such as inhalers, tablets, or oxygen therapy) exactly as directed by your healthcare team.
– Lifestyle changes and breathing techniques are designed to support your care, not replace your medicines.
– If you notice your symptoms getting worse – such as needing your reliever inhaler more often, increased breathlessness, or more mucus production – contact your GP, asthma/COPD nurse, or healthcare team promptly.
– If you have an acute flare-up (for example, severe breathlessness, chest tightness, or difficulty speaking in sentences), follow your personal action plan. If symptoms do not improve quickly, call 111 in the UK (or your local urgent care service).
– Call 999 immediately if you have severe breathlessness at rest, blue lips/fingers, confusion, or if you are unable to speak more than a few words. These are signs of a medical emergency.
Always speak to your healthcare provider before making major changes to your diet, exercise, or supplement routine – especially if you have other health conditions or take regular medication.
- Archana Dhengare and Savita Pohekar (2021) “To Assess the Effectiveness of Selected Breathing Exercises among Chronic Obstructive Pulmonary Disease Patients”, Journal of Pharmaceutical Research International, 33(54B), pp. 354–361. doi: 10.9734/jpri/2021/v33i54B33798.
- Arora, Rachna & Dhokpatil, Shruti & Verma, Chhaya & Rajadhyaksha, Girish. (2022). Effect of Buteyko Breathing Technique on Haemodynamic Parameters and Functional Capacity in Subjects with Primary Hypertension. Indian Journal of Physiotherapy & Occupational Therapy – An International Journal. 16. 73-80. 10.37506/ijpot.v16i3.18400.
- Association of Chartered Physiotherapists in Respiratory Care, (2011), The Active Cycle of Breathing Techniques.
- Baig, Bilal & Anwar, Mamaoona & Rasheed, Maryam & Rasul, Akhtar & Fiaz, Aiman & Faisal, Sidra. (2024). Comparative Effects of Buteyko Breathing Technique and Active Cycle of Breathing Technique on Dyspnea and Quality of Life in Patients with Chronic Obstructive Pulmonary Disease. Journal of Health and Rehabilitation Research. 4. 250-255. 10.61919/jhrr.v4i1.192.
- Bott, J., S Blumenthal, M Buxton, S Ellum, C Falconer, R Garrod, A Harvey, T Hughes,
- British Lung Foundation, Singing for Lung Health.
- Bruton, Anne & Lee, Amanda & Yardley, Lucy & Raftery, James & Arden-Close, Emily & Kirby, Sarah & Zhu, Shihua & Thiruvothiyur, Manimekalai & Webley, Frances & Taylor, Lyn & Gibson, Denise & Yao, Guiqing & Stafford-Watson, Mark & Versnel, Jenny & Moore, Michael & George, Steve & Little, Paul & Djukanovic, Ratko & Price, David & Thomas, Mike. (2017). Physiotherapy breathing retraining for asthma: A randomised controlled trial. The Lancet Respiratory Medicine. 6. 10.1016/S2213-2600(17)30474-5.
- BTS/NICE/SIGN Joint Guideline on Asthma: diagnosis, monitoring and chronic asthma management.
- Budiono, Budiono & Mustayah, Mustayah & Aindrianingsih,. (2019). THE EFFECT OF PURSED LIPS BREATHING IN INCREASING OXYGEN SATURATION IN PATIENTS WITH CHRONIC OBSTRUCTIVE PULMONARY DISEASE IN INTERNAL WARD 2 OF THE GENERAL HOSPITAL OF DR. R. SOEDARSONO PASURUAN. Public Health of Indonesia. 3. 10.36685/phi.v3i3.132.
- Charikiopoulou, Maria & Nikolaidis, Pantelis & Knechtle, Beat & Rosemann, Thomas & Rapti, Aggeliki & Trakada, Georgia. (2019). Subjective and Objective Outcomes in Patients With COPD After Pulmonary Rehabilitation – The Impact of Comorbidities. Frontiers in Physiology. 10. 10.3389/fphys.2019.00286.
- Chen Y, Li P, Wang J, Wu W, Liu X. Assessments and Targeted Rehabilitation Therapies for Diaphragmatic Dysfunction in Patients with Chronic Obstructive Pulmonary Disease: A Narrative Review. Int J Chron Obstruct Pulmon Dis. 2022 Mar 3;17:457-473. doi: 10.2147/COPD.S338583. PMID: 35273448; PMCID: PMC8902058.
- Clark, Imogen & Harding, Katherine. (2012). Psychosocial outcomes of active singing interventions for therapeutic purposes: A systematic review of the literature. Nordic Journal of Music Therapy. 21. 80-98. 10.1080/08098131.2010.545136.
- Critchley, Hugo & Nicotra, Alessia & Chiesa, Patrizia & Nagai, Yoko & Gray, Marcus & Minati, Ludovico & Bernardi, Luana. (2015). Slow Breathing and Hypoxic Challenge: Cardiorespiratory Consequences and Their Central Neural Substrates. PloS one. 10. e0127082. 10.1371/journal.pone.0127082.
- Global Initiative for Chronic Obstructive Lung Disease (2023), Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease.
- Greenwell, K., Ainsworth, B., Bruton, A. et al. Mixed methods process evaluation of my breathing matters, a digital intervention to support self-management of asthma. npj Prim. Care Respir. Med. 31, 35 (2021).
- Hariyono, Rudi & Santoso, Dwi & Arsa, Putu & Rozi, Fahrur. (2017). The Influence of Pursed Lip Breathing on Dyspnea, Oxygen Saturation and Activity Tolerance on COPD Patient:Systematic Review. 10.2991/inc-17.2017.15.
- Hassan EEM, Abusaad FE, Mohammed BA. Effect of the Buteyko breathing technique on asthma severity control among school age children. Egypt J Bronchol. 2022;16(1):45. doi: 10.1186/s43168-022-00149-3. Epub 2022 Jul 23. PMCID: PMC9308119.
- https://www.health.harvard.edu/staying-healthy/understanding-the-stress-response.
- https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/baroreflex.
- Huang J, Yuan X, Zhang N, Qiu H, Chen X. Music Therapy in Adults With COPD. Respir Care. 2021 Mar;66(3):501-509. doi: 10.4187/respcare.07489. Epub 2020 Nov 3. PMID: 33144384.
- Hussain, Muhammad & Sheraz, Suman & Razzaq, Aisha & Malik, Arshad. (2022). Active Cycle of Breathing Techniques Improves Post-operative Pulmonary Complications in Coronary Artery Bypass Graft Surgery Patients. 55. 186-190.
- Kaasgaard M, Rasmussen DB, Løkke A, Vuust P, Hilberg O, Bodtger U. Physiological changes related to 10 weeks of singing for lung health in patients with COPD. BMJ Open Respir Res. 2022 May;9(1):e001206. doi: 10.1136/bmjresp-2022-001206. PMID: 35545297; PMCID: PMC9096537.
- Karunarathne, Udani & Amarasiri, D Lakmali & Fernando, Anne. (2023). Respiratory function in healthy long-term meditators: A cross-sectional comparative study. Heliyon. 9. e18585. 10.1016/j.heliyon.2023.e18585.
- Lewis A, Philip KEJ, Lound A, Cave P, Russell J, Hopkinson NS. The physiology of singing and implications for ‘Singing for Lung Health’ as a therapy for individuals with chronic obstructive pulmonary disease. BMJ Open Respiratory Research. 2021;8:e000996.
- Lewis, Adam, Phoene Cave, Nicholas S Hopkinson, (2017) Singing for Lung Health: a qualitative assessment of a British Lung Foundation programme for group leaders, BMJ Open Respiratory Research.
- Lincoln, M. C Mikelsons, C Potter, J Pryor, L Rimington, F Sinfield, C Thompson,
- Lord VM, Cave P, Hume VJ, Flude EJ, Evans A, Kelly JL, Polkey MI, Hopkinson NS. Singing teaching as a therapy for chronic respiratory disease–a randomised controlled trial and qualitative evaluation. BMC Pulm Med. 2010 Aug 3;10:41. doi: 10.1186/1471-2466-10-41. PMID: 20682030; PMCID: PMC2920262.
- McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015 Feb 23;2015(2):CD003793. doi: 10.1002/14651858.CD003793.pub3. PMID: 25705944; PMCID: PMC10008021.
- McNaughton A, Weatherall M, Williams M, et al, Sing Your Lungs Out – a community singing group for chronic obstructive pulmonary disease: a 1-year pilot study. BMJ Open 2017;7:e014151.
- Mendes, Liliane & Moraes, Karoline & Hoffman, Mariana & Vieira, Danielle & Ribeiro-Samora, Giane & Lage, Susan & Britto, Raquel & Parreira, Verônica. (2018). Effects of Diaphragmatic Breathing With and Without Pursed-Lips Breathing in Subjects With COPD. Respiratory Care. 64. respcare.06319. 10.4187/respcare.06319.
- Mohamed, Yosreah & Elderiny, Sabah & Mohamed, Lobna. (2019). The effect of Buteyko breathing technique among patients with bronchial asthma: Comparative study. International Journal of Midwifery and Nursing Practice. 2. 01-10. 10.33545/26630427.2019.v2.i2a.36.
- Morrow, Brenda & Brink, Jarred & Grace, Samantha & Pritchard, Lisa & Lupton-Smith, Alison. (2016). The effect of positioning and diaphragmatic breathing exercises on respiratory muscle activity in people with chronic obstructive pulmonary disease. South African Journal of Physiotherapy. 72. 10.4102/sajp.v72i1.315.
- Mulyadi, & Junita, Ida & Zulfikar, Teuku & Yusuf, Nurrahmah & Azhary, Mulkan & Salim, Hotimah. (2022). The effect of pursed-lips breathing and diaphragm exercises on the quality of life of COPD patient assessed by six-minutes walk test. Bali Medical Journal. 11. 1116-1120. 10.15562/bmj.v11i3.3474.
- NHS. (2023) COPD Treatment.
- NICE, (2019) NG115.
- Parkavi, K & Umarani, R & Anusha, N & Rashika, R. (2022). Effect of Pursed Lip Breathing on Physiological Cost Index and Functional Exercise Capacity in Patients with Chronic Obstructive Pulmonary Disease. YMER Digital. 21. 247-254. 10.37896/YMER21.03/28.
- Pathan, Anam & Yadav, Vaishnavi & Jain, Moli & Saifee, Sakina. (2022). An Early Comprehensive Physiotherapy Approach towards Reconditioning of Patient with Empyema Thoracis: A Case Study. Journal of Pharmaceutical Research International. 10.9734/jpri/2021/v33i59B34358.
- Pfab, F., Schalock, P.C., Napadow, V., Athanasiadis, G.I., Ring, J. and Huss-Marp, J. (2013), Review. Focus on Alternative and Complementary Therapies, 18: 77-84.
- Phillips, Jennifer & Lee, Annemarie & Pope, Rod & Hing, Wayne. (2021). Physiotherapists’ use of airway clearance techniques during an acute exacerbation of bronchiectasis: a survey study. Archives of Physiotherapy. 11. 3. 10.1186/s40945-020-00097-5.
- Pierobon, Antonia & Bottelli, Elisa & Ranzini, Laura & Bruschi, Claudio & Maestri, Roberto & Bertolotti, Giorgio & Sommaruga, Marinella & Torlaschi, Valeria & Callegari, Simona & Giardini, Anna. (2017). COPD patients’ self-reported adherence, psychosocial factors and mild cognitive impairment in pulmonary rehabilitation. International Journal of Chronic Obstructive Pulmonary Disease. 12. 2059-2067. 10.2147/COPD.S133586.
- Prakash, Jayabalan & James, Tittu Thomas & Menaria, Shubham & Usman, Anas & John, Centina. (2021). Effectiveness of short-term belly breathing training in individuals who work-from-home during the COVID-19 lockdown in India. International Journal of Research in Pharmaceutical Sciences. 12. 2014-2019. 10.26452/ijrps.v12i3.4809.
- Prem V, Sahoo RC, Adhikari P. Comparison of the effects of Buteyko and pranayama breathing techniques on quality of life in patients with asthma – a randomized controlled trial. Clin Rehabil. 2013 Feb;27(2):133-41. doi: 10.1177/0269215512450521. Epub 2012 Jul 26. PMID: 22837543.
- Qureshi, Muskan & Lalwani, Lajwanti & Aherrao, Samruddhi. (2024). The Role of Chest Physiotherapy in Enhancing Quality of Life in a Postoperative Patient With Gingivobuccal Sulcus Carcinoma and Empyema: A Case Report. Cureus. 16. 10.7759/cureus.70492.
- Rahmad, Rahmad & Narasati, Shabrina & NUGROHO, EKO & WITJAKSONO, DJOKO & LESTARI, DWI & NUGROHO, M. & RACHMAWATI, SAMIAH & RIDWAN, M.. (2020). THE ROLE OF PULMONARY REHABILITATION IN ACUTE EXACERBATIONS OF CHRONIC OBSTRUCTIVE PULMONARY DISEASE. International Journal of Applied Pharmaceutics. 39-40. 10.22159/ijap.2020.v12s3.39466.
- Rahmi, Upik & Susanto, Herry & Krzyż, Ewa & Widiyaningsih, Widiyaningsih. (2023). Effect of Pursed lip Breathing Exercise to Reduce Dyspnea in Patient with Asthma Bronchial: Case Study. JURNAL PENDIDIKAN KEPERAWATAN INDONESIA. 8. 113-118. 10.17509/jpki.v8i2.51803.
- Ritz, T. David Rosenfield, Ashton M Steele, Mark W Millard, Alicia E Meuret, Controlling Asthma by Training of Capnometry-Assisted Hypoventilation (CATCH) vs Slow Breathing: A Randomized Controlled Trial, Chest, Volume 146, Issue 5, 2014, Pages 1237-1247, ISSN 0012-3692.
- Roberts, S. & Schreuder, Fiona & Watson, Tim & Stern, Madison. (2012). The long-term experience of COPD patients taught PLB: a mixed methodological study.. Thorax. 67. A107. 10.1136/thoraxjnl-2012-202678.384.
- Salomoni, Sauro & van den Hoorn, Wolbert & Hodges, Paul. (2016). Breathing and Singing: Objective Characterization of Breathing Patterns in Classical Singers. PloS one. 11. e0155084. 10.1371/journal.pone.0155084.
- Sankar U, Ganapathy & R., Monisha & Vallabadoss, Christopher Amalraj & R M, Palanivel. (2020). Efficacy of breathing retraining program on bedside assessment of pulmonary function. International Journal of Research in Pharmaceutical Sciences. 11. 1467-1471. 10.26452/ijrps.v11i2.2019.
- Sartika, Andry & Andri, Juli & Padila, Padila. (2022). Progressive Muscle Relaxation (PMR) Intervention with Slow Deep Breathing Exercise (SDBE) on Blood Pressure of Hypertension Patients. JOSING: Journal of Nursing and Health. 2. 65-76. 10.31539/josing.v2i2.3485.
- Sawitri, Atri & Yuniarti, Enny & Pratiwi, Rizky. (2024). Active Cycle of Breathing Technique (ACBT) and Effective Coughing on Respiratory Rate Changes in COPD Patients. JENDELA NURSING JOURNAL. 8. 145-151. 10.31983/jnj.v8i2.12000.
- Vaughn, P. J White, (2009), Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient, Thorax 64;(Suppl I):i1–i51. doi:10.1136/thx.2008.110726.
- Udayani, Wiwik & Amin, Muhammad & Makhfudli, Makhfudli. (2019). The Effect of Combination of Buteyko Breathing Technique and Walking Exercise on Forced Peak Expiratory Flow In Adult Asthmatic Patients. Jurnal Keperawatan Padjadjaran. 7. 10.24198/jkp.v7i2.1193.
- Zhang, Hong & Hu, Dandan & Xu, Yikai & Wu, Lixia & Lou, Liming. (2022). Effect of pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis of randomized controlled trials. Annals of Medicine. 54. 262-273. 10.1080/07853890.2021.1999494.





