Managing asthma or COPD isn’t just about your lungs – it’s about your whole life.
When you live with asthma or COPD, it can sometimes feel like your life is ruled by your lungs. Inhalers, peak flows, flare-ups – these all matter. But science is clear: your breathing is not only about your lungs. Emotional wellbeing, stress, anxiety, mood, social support, and even how you think about your illness can make a real difference to how well you breathe and how confident you feel, managing your condition day to day.
In this article, we’ll explore psychological and mind-body strategies that have been shown to help people with long-term lung conditions. These don’t replace medicines or medical care, but they can sit alongside them, giving you extra tools to manage symptoms and improve your quality of life.
Stress, emotions, and breathing

When breathlessness strikes, fear usually follows. That fear can then make breathing harder – setting up what researchers call a self-reinforcing loop. This can worsen symptoms through multiple pathways:
- Hyperventilation (fast, shallow breathing) or panic can trigger breathlessness
- Anxiety and stress increase awareness of normal respiratory sensations, making them feel more threatening
- Depression can reduce motivation to take medicines, stay active, or reach out for help
- Social isolation can increase risk of hospitalisation and lower quality of life
Research shows that depression is around two to three times more common in people with COPD than in the general population, and anxiety affects up to half of people with asthma. These emotional challenges are linked to more flare-ups, higher healthcare use, and reduced quality of life.
What’s especially interesting is that the relationship seems to work both ways. Some studies suggest asthma may increase the risk of anxiety or depression, while in other cases mental health problems appear first and increase the chance of asthma symptoms later. This shows just how connected the mind and body are.
Why this matters: It’s not “just in your head.” Emotional health directly affects your physical symptoms. Recognising this link builds capability (“I understand what’s happening”), motivation (“I can do something about it”), and opportunity (“there are tools available”).
The body-mind connection: emerging science
Stress doesn’t just change how you feel – it can also affect what’s happening inside your body. Newer research shows that psychological stress can make the immune system more reactive, raising inflammation in the lungs.
In asthma, short bursts of stress in the lab have been shown to increase inflammatory markers, while long-term stress may even reduce how well steroids work to calm down airway inflammation.
In COPD, flare-ups are strongly linked to spikes in inflammatory and oxidative stress markers, and there is growing interest in how emotional stress might play a part in tipping people into these episodes.
The science is still evolving, but it supports what many people notice day to day: stress makes breathing feel worse. This means that looking after your emotional wellbeing isn’t just about feeling calmer – it may also protect your lungs from unnecessary flare-ups.
Managing fear during an asthma or COPD attack:
It’s natural to feel panicked during an asthma flare-up or COPD exacerbation – shortness of breath and tightness can trigger intense fear – and that fear often makes breathing even harder.
Research shows that learning simple breathing techniques like slow diaphragmatic breathing and pursed-lip breathing can reduce anxiety, calm your nervous system, and help you regain breath control.
Techniques taught in Cognitive Behavioural Therapy (CBT) – such as recognising unhelpful thoughts, using relaxation strategies, and gradually confronting breathlessness – can prevent panic attacking your symptoms and improve your confidence with breathing.
In people with COPD, these approaches have been shown to limit activity avoidance, lift mood, and reduce flare-ups of breathlessness-linked anxiety (Yang et al., 2020; Burge et al., 2024).
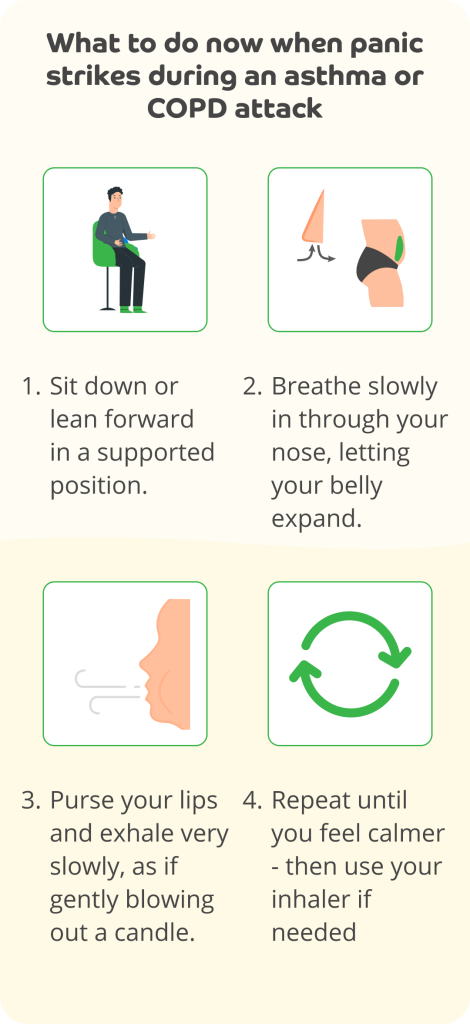
Practising these steps regularly outside of attacks (e.g., daily), reduces fear in future episodes and gives you a tool to regain composure when breathlessness hits.
Recognising and addressing emotional health is a core part of asthma and COPD care in both NICE and BTS/SIGN guidelines.
Cognitive Behavioural Therapy (CBT): changing unhelpful thoughts

CBT is a talking therapy that helps people notice and change unhelpful thoughts and behaviours. In asthma and COPD, it can:
- Reduce fear of flare-ups.
- Break the cycle of panic and breathlessness.
- Improve mood and confidence in self-management.
A systematic review found CBT improved anxiety, depression, and quality of life in people with COPD. NICE also recommends CBT referral if anxiety or depression are making asthma symptoms worse.
🟩 Try it yourself: CBT “thought check”
- Notice the first thought when symptoms appear.
- Ask: Is this thought helping me or making things worse?
- Challenge it: What’s the evidence this will last forever?
- Replace it: “This is scary, but I know how to manage it.”
- Write down one “unhelpful thought” and one “balanced thought” each day.
How to access CBT:
– Ask your GP for referral to NHS Talking Therapies.
– Some pulmonary rehabilitation programmes include
– NHS-approved online CBT platforms may be available.
🧘 Mindfulness and meditation

Mindfulness means paying attention to the present moment in a kind, non-judgemental way. It’s been shown to:
- Reduce stress and anxiety.
- Improve coping with breathlessness.
- Support quality of life, even if lung function doesn’t change.
In asthma, an 8-week mindfulness course improved wellbeing and stress levels. In COPD, reviews show promise in supporting both mood and physical outcomes.
🟩 Try it yourself: 2-minute mindful breath
- Sit comfortably and close your eyes.
- Notice your breath moving in and out of your nose.
- If your mind wanders, gently bring it back to the breath.
- Continue for 2 minutes. Increase over time if helpful.
Other approaches such as Acceptance and Commitment Therapy (ACT) aim to help people live well alongside symptoms. Early studies suggest ACT may reduce avoidance behaviours and support wellbeing.
Mindfulness apps (like Headspace or Insight Timer) or structured Mindfulness Based Stress Reduction (MBSR) courses may be helpful additions to usual care.
Relaxation strategies
Simple relaxation exercises, such as progressive muscle relaxation, can reduce stress hormones and lower the perception of breathlessness.
🟩 Try it yourself: Progressive muscle relaxation
- Sit or lie down comfortably.
- Starting with your feet, tense the muscles for 5 seconds, then release.
- Move slowly up the body: calves, thighs, stomach, shoulders, face.
- Notice the difference between tension and relaxation.
🎵 Singing, art, and creative therapies

Creative therapies like art and music may also help express emotions and reduce stress. Creative therapies help people express themselves, connect with others, and engage in joyful activities that support breathing control.
Singing for Lung Health groups use music to strengthen breathing muscles, improve posture, and build confidence. People also report better mood and less isolation.
🟩 Try it yourself: Singing for breath
- Choose a song you enjoy.
- Take a deep belly breath before each line.
- Focus on a steady, gentle out-breath as you sing.
Ask your respiratory team about local or online options. Some groups now run virtual sessions for accessibility.
🤝 Social support and peer connection
Asthma and COPD can feel isolating, but support makes a huge difference.
If you have asthma, support from friends, family, or a group can make it easier to stay on top of your medicines, keep active, and cope with flare-ups. Knowing you’re not managing it alone can reduce stress and even lower the chance of urgent care visits.
Talking with others who understand asthma – whether in a local group or an online community – can boost your confidence, give you practical tips, and help you feel less isolated.
Just as support makes a real difference for people with asthma, it’s equally – if not more – important in COPD, where staying connected can help you manage day-to-day challenges and cope with the ups and downs of the condition. Peer-led COPD programmes have been shown to reduce hospital admissions and improve confidence. Strong social networks are linked to better medication use, faster recovery, and lower stress.
Some research suggests that spirituality or religious belief can also help people cope with COPD by reducing distress and providing meaning. This won’t apply to everyone, but it highlights how diverse coping strategies can be.
Living with COPD can bring up fears about the future – worries about your health getting worse, losing independence, or even thoughts about death. These feelings are natural, but they can add to the distress you already feel. Talking openly with people you trust, including your healthcare team, about these fears can ease the burden and may help you feel more supported and improve your quality of life.
🟩 Try it yourself: Build a support plan
- Write down two people you can contact when you feel low or anxious.
- Ask your GP or search online for local support groups such as Breathe Easy groups: All Breathe Easy groups | Asthma + Lung UK
- Set a weekly “social goal”: a call, group, or online forum.
Summary: Mind-body strategies you can try
Looking after your mind is part of looking after your lungs. NICE, BTS and SIGN guidelines all highlight emotional wellbeing as an essential part of care.
- CBT has the strongest evidence. Helps reduce anxiety and depression, builds confidence, and breaks the cycle of panic and breathlessness.
- Mindfulness and ACT show moderate benefits. Calms the mind, reduce stress, and support living well with symptoms. Easy to try with short daily practices or apps.
- Breathing and relaxation provides simple, practical tools. Quick to learn, calm the nervous system, and give you control during flare-ups.
- Singing and creative therapies are growing areas with positive results. Supports breathing, lifts mood, and reduces isolation – and they’re enjoyable to do.
- Social support and meaning are vital but often overlooked. Strong networks, groups, or personal beliefs improve confidence, reduce stress, and help you feel less alone.
Managing your emotional health isn’t “extra” – it’s a proven way to improve your breathing, your confidence, and your quality of life. Even small steps – one new skill, one new group, or one daily practice – can make a real difference to your breathing and wellbeing.
If you haven’t already, download the free Evergreen Life app to track your health, including managing your asthma and/or COPD, and get practical tips that help you take control of your overall health.
This article is intended for educational purposes only and is designed to support adults (aged 18 and over) living with asthma, COPD, or asthma-COPD overlap. It does not replace individual medical advice, mental health care, or prescribed treatments. Please consult a qualified healthcare professional before making changes to your treatment plan or mental health support.
Mind-body strategies – including breathing techniques, relaxation, mindfulness, and psychosocial support – can play a helpful role in reducing anxiety, improving quality of life, and supporting better symptom control. However, these approaches are adjunctive and should always be used alongside, not instead of, medical treatments for asthma or COPD.
If you are experiencing:
– Persistent anxiety, low mood, or distress related to your breathing condition
– Difficulty managing your symptoms despite treatment
– Feelings of isolation or disconnection
– Night-time panic related to breathlessness
– Avoidance of activities due to fear of flare-ups
– Changes in sleep, appetite, concentration, or daily functioning
Please speak to your GP, nurse, or mental health professional. Psychological wellbeing is an important part of your overall health and support is available.
If you are in crisis or need urgent mental health support:
– Contact your GP or call NHS 111 for advice
– Call Samaritans free on 116 123 (available 24/7 in the UK)
– In an emergency or if you are at risk of harm, call 999 or attend A&E
Medical safety
– If you are having an asthma or COPD flare-up, or your breathlessness suddenly worsens, follow your personal action plan and seek urgent medical advice if needed
– Never stop prescribed medication (including preventers, relievers, or tablets) without discussing with your clinical team
– If you notice mental health changes after starting a new medication (e.g. montelukast), report symptoms promptly to your GP or via the MHRA Yellow Card scheme
Mind-body strategies can support your breathing journey – but they work best when integrated safely with your wider care plan. Your clinical team is here to help you find the right balance.
- Bramanti, A., Pessolano, C., Garofano, M., Maglio, A. A., Ciccarelli, M., Budaci, L., Calabrese, M., Marino, A., Loria, F., Corallo, F., Bramanti, P., Vecchione, C., & Vatrella, A. (2025). Mindfulness-Based Interventions for Chronic Pulmonary Diseases: A Systematic Review of Effects on Anxiety, Depression, Stress, Dyspnea, and Quality of Life. Bioengineering, 12(9), 931.
- Brighton, Lisa. (2023) Mental health and COPD: Why we need more research, Asthma + Lung UK.
- British Lung Foundation, Singing for lung health.
- Burge AT, Gadowski AM, Jones A, Romero L, Smallwood NE, Ekström M, Reinke LF, Saggu R, Wijsenbeek M, Holland AE. Breathing techniques to reduce symptoms in people with serious respiratory illness: a systematic review. Eur Respir Rev. 2024 Oct 30;33(174):240012. doi: 10.1183/16000617.0012-2024. PMID: 39477355; PMCID: PMC11522968.
- Effing TW, Bourbeau J, Vercoulen J, Apter AJ, Coultas D, Meek P, Valk Pv, Partridge MR, Palen Jv. Self-management programmes for COPD: moving forward. Chron Respir Dis. 2012 Feb;9(1):27-35. doi: 10.1177/1479972311433574. PMID: 22308551.
- Giusti EM, Papazian B, Manna C, Giussani V, Perotti M, Castelli F, Battaglia S, Galli P, Rossi A, Re V, Goulene K, Castelnuovo G, Stramba-Badiale M. The Effects of an Acceptance and Commitment-Informed Interdisciplinary Rehabilitation Program for Chronic Airway Diseases on Health Status and Psychological Symptoms. Front Psychol. 2022 Jan 27;12:818659. doi: 10.3389/fpsyg.2021.818659. Erratum in: Front Psychol. 2023 Mar 07;14:1168593. doi: 10.3389/fpsyg.2023.1168593. PMID: 35153934; PMCID: PMC8828560.
- GOLD, (2024) 2024 Gold Report.
- Goldin, James, Florence Bodeau-Livinec, Dietmar Goelitz, Adina Bitfoi, Mauro Giovanni Carta, Ceren Koç, Sigita Lesinskiene, Zlatka Mihova, Roy Otten, Viviane Kovess-Masfety, The association between mental health problems and asthma among European school children, The European Journal of Psychiatry, Volume 37, Issue 4, 2023, 100223, ISSN 0213-6163.
- IPCRG (2022) COPD and Mental Health: Holistic and Practical Guidance for Primary Care.
- Kotlińska-Lemieszek A, Fopka-Kowalczyk M, Krajnik M. Spirituality in people with advanced chronic obstructive pulmonary disease – challenge for more effective interventions, support, and healthcare education: Mini-review. Front Med (Lausanne). 2022 Dec 6;9:954519. doi: 10.3389/fmed.2022.954519. PMID: 36561722; PMCID: PMC9763313.
- Liu, Xiaoqin et al. Bidirectional Associations Between Asthma and Types of Mental Disorders. The Journal of Allergy and Clinical Immunology: In Practice, Volume 11, Issue 3, 799 – 808.e14
- Maritescu A, Crisan AF, Pescaru CC, Oancea C, Iacob D. The Psychological and Physical Benefits of Progressive Muscle Relaxation in Chronic Respiratory Diseases: A Systematic Review. Medicina (Kaunas). 2025 Jun 7;61(6):1055. doi: 10.3390/medicina61061055. PMID: 40572743; PMCID: PMC12195441.
- NICE, (2024) Asthma: diagnosis, monitoring and chronic asthma management (BTS, NICE, SIGN). NG245. NICE.
- Opozda, Melissa & Wilson, Ian. (2005). Asthma and depression: A pragmatic review of the literature and recommendations for future research. Clinical practice and epidemiology in mental health : CP & EMH. 1. 18. 10.1186/1745-0179-1-18.
- Oren, Eyal et al. Stress and asthma. Annals of Allergy, Asthma & Immunology, Volume 125, Issue 4, 372 – 373.e1.
- Palumbo, María Laura & Prochnik, Andrés & Wald, Miriam Ruth & Genaro, Ana María. (2020). Chronic stress and glucocorticoid receptor resistance in asthma. Clinical Therapeutics. 42(6). 993–1003. 10.1016/j.clinthera.2020.04.016.
- Pbert L, Madison JM, Druker S, Olendzki N, Magner R, Reed G, Allison J, Carmody J. Effect of mindfulness training on asthma quality of life and lung function: a randomised controlled trial. Thorax. 2012 Sep;67(9):769-76. doi: 10.1136/thoraxjnl-2011-200253. Epub 2012 Apr 27. PMID: 22544892; PMCID: PMC4181405.
- Wang J, Willis K, Barson E, Smallwood N. The complexity of mental health care for people with COPD: a qualitative study of clinicians’ perspectives. NPJ Prim Care Respir Med. 2021 Jul 22;31(1):40. doi: 10.1038/s41533-021-00252-w. PMID: 34294727; PMCID: PMC8298614.
- Williams MT, Johnston KN, Paquet C. Cognitive Behavioral Therapy for People with Chronic Obstructive Pulmonary Disease: Rapid Review. Int J Chron Obstruct Pulmon Dis. 2020 Apr 23;15:903-919. doi: 10.2147/COPD.S178049. PMID: 32425516; PMCID: PMC7186773.
- Yang Y, Wei L, Wang S, Ke L, Zhao H, Mao J, Li J, Mao Z. The effects of pursed lip breathing combined with diaphragmatic breathing on pulmonary function and exercise capacity in patients with COPD: a systematic review and meta-analysis. Physiother Theory Pract. 2022 Jul;38(7):847-857. doi: 10.1080/09593985.2020.1805834. Epub 2020 Aug 18. PMID: 32808571.
- Yohannes AM, Alexopoulos GS. Depression and anxiety in patients with COPD. Eur Respir Rev. 2014 Sep;23(133):345-9. doi: 10.1183/09059180.00007813. PMID: 25176970; PMCID: PMC4523084.
- Zinellu E, Zinellu A, Fois AG, Pau MC, Scano V, Piras B, Carru C, Pirina P. Oxidative Stress Biomarkers in Chronic Obstructive Pulmonary Disease Exacerbations: A Systematic Review. Antioxidants (Basel). 2021 Apr 29;10(5):710. doi: 10.3390/antiox10050710. PMID: 33946941; PMCID: PMC8146706.





