Right now, your gut microbiome is a hive of activity with trillions of microbes such as bacteria, fungi, and viruses influencing how your body functions.
A healthy gut, like a healthy rainforest, is one with high microbial diversity. In contrast, an unhealthy gut is often referred to being in a state of dysbiosis. This means there’s an imbalance in the gut microbiome, which could be down to gaining or losing a certain species of microbe or changes in the relative abundance of microbes, making you more susceptible to harmful bacteria and disease.
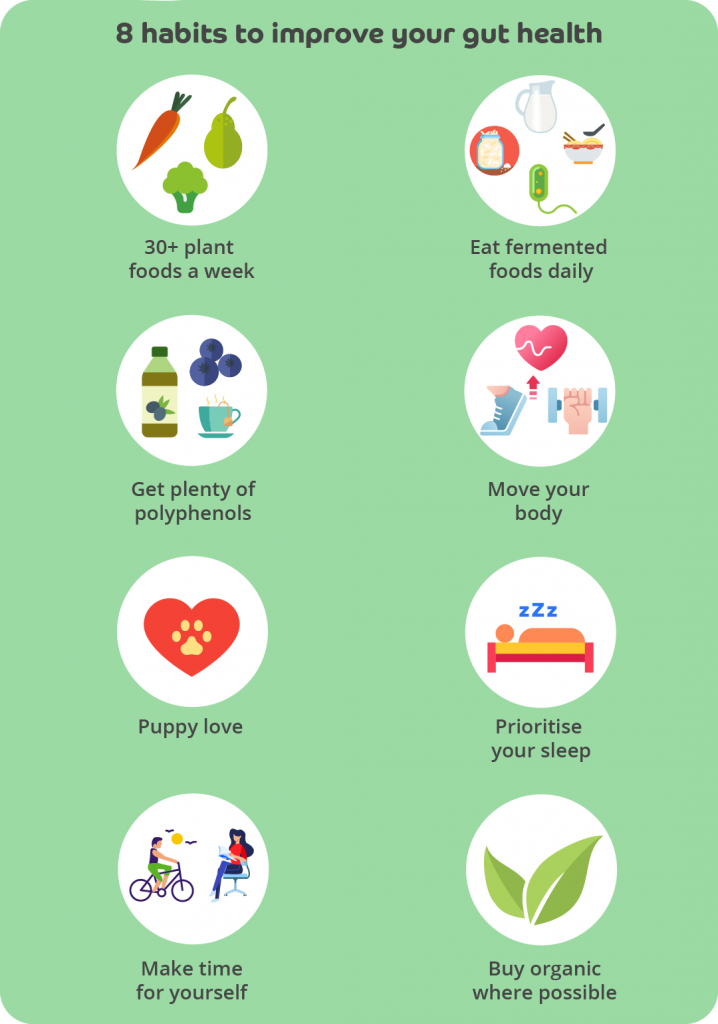
Below we outline a variety of factors that can trigger some level of disruption to this collection of bugs. You can then take action if you like to restore more balance and support your gut health. The ways you can restore balance to your gut microbiome are summarised in our graphic and at the end and you can discover more in our other articles.
Jump to section
What factors affect your gut microbiome?
Disruptors you can’t control:
Being born by caesarean section

A healthy human foetus is traditionally thought to develop in an bacteria-free environment, meaning the gut of a healthy unborn baby is sterile, although more recent evidence suggests the placenta may contain its own microbiome that contributes to the make-up of a baby’s gut microbiome. Nevertheless, it’s generally accepted the mother’s vaginal microbiome (along with her gut microbiome) are the primary sources of microbes that make up the baby’s gut microbiome, with microbes transferred from the mother’s vaginal microbiome to the baby during vaginal birth.
The mother’s vaginal and gut microbiomes change during pregnancy, and this is likely to be part of an adaptive response to protect and promote the health of the unborn baby and provide the newborn with specific protective microbes at birth, before exposure to other environmental microbes.
How?
Babies born via caesarean section don’t have this exposure to the vaginal microbiome and their gut microbiomes are more likely to include skin and oral microbes and even bacteria from the operating room. Compared to being born naturally, caesarean babies are more likely to have a slower diversifying gut microbiome.
Children born via caesarean are more likely to develop asthma and allergies and the microbiome differences persist even in adulthood. Studies have even shown a moderate association between children born via caesarean delivery and obesity. Other research indicates caesarean delivery may increase the likelihood of the baby developing coeliac disease and Type 1 diabetes.
How long does the disruption last?
One study revealed that the gut bacteria in caesarean babies may be disturbed for up to six months after the birth, whilst another study indicated the disruption may continue for up to seven years. However long the disruption lasts, it remains unclear whether differences in microbiome as a result of vaginal and caesarean births cause any disease-related problems in adults. Whilst you can’t help if you were born via caesarean section – a procedure that’s usually unavoidable – lifestyle changes can support the composition of your gut microbiome as an adult.
Ways to potentially restore caesarean babies’ microbiomes

Studies over the last few years have found that exposing newborns delivered by caesarean section to maternal vaginal fluids at birth, a practice known as “vaginal seeding”, enriched their gut, oral and skin microbiomes akin to that of a baby born naturally in the first 30 days of life.
More recently, orally delivered faecal microbiota transplantation (FMT) from the mother has been put forward as the most natural and cost-effective way to restore the gut microbiomes of full-term infants delivered by caesarean section. Specifically, maternal FMT corrected the delayed Bifidobacterium development and the lack of the gut bacteria called Bacteroides in c-section delivered babies, that often characterise the microbiomes of caesarean infants. In fact, the transplanted caesarean section-born infants showed normal faecal microbiome development. Notably, the study found that vaginal seeding didn’t correct the c-section-induced microbiome imbalance.
The results of a trial investigating the oral administration of maternal vaginal microbes at birth to restore the gut microbiome development in c-section infants involving 47 mothers and babies also led the researchers to conclude that exposure to the maternal faecal, rather than vaginal, microbiome may be a more effective method for restoring Bacteroides levels in babies born by caesarean section.
Not being breastfed

Over the first three years of life, the microbiome evolves from relatively simple but rapidly increasing in diversity to an adult state that’s more complex and stable. Breastmilk provides prebiotics that support the development of the baby’s microbiome by feeding the beneficial gut microbes.
It also contains a diverse array of microbes – with one study identifying up to 820 species. As we’ve established, a healthy gut tends to be one with a diverse microbial community, although the functional significance of human milk bacteria remains unclear. Intriguingly, one study found faecal diversity was lower in breast-fed infants than formula-fed ones in their early life but increased significantly when they started eating solid foods. A low diversity of the gut microbes in early life seemed to characterise a healthy gut, if caused by breastfeeding, which differs from theories about adults.
So, bottle feeding produces a more varied microbiome than breastfeeding, but evidence is strong that it’s associated with poorer health later in life. We don’t know, however, whether that outcome is related to the microbiome change.
What’s clear is that bacteria in breastmilk contributes to the overall make-up of a baby’s microbiome as one study detected the same species of a few bacteria in the mothers’ milk and their infant’s stool. The same study found that the number of bacteria the mother’s milk and baby’s stool have in common is reduced when the breastmilk is pumped and given to the baby via a bottle than from the breast directly.
Another bonus for breastfeeding
Fascinatingly, one small study also revealed that breastfeeding has the potential to restore the delayed gut microbiome development of caesarean-born infants to that of babies born naturally.
How?
A longitudinal 12-month study of 107 healthy pairs of mothers and babies found that breastfed infants received 27.7% of their gut bacteria from breastmilk as you might expect. Fascinatingly though, they also received 10.4% from the skin around the mother’s areola during the first month of life, highlighting another benefit of breastfeeding directly if possible.
Genetics

Despite gut microbiomes being unique to each individual, relatives often have more similar microbiomes than unrelated people. Biological families are genetically similar and often share a common environment, for example, eating the same type of food. So, this similarity could be both genetic and environmental.
An example of the genetic influence on our microbiome is illustrated by what we know about one of the most highly heritable gut bacteria family Christensenellaceae, which is associated with a reduction of BMI. The human genotype (complete set of genetic material) is estimated to influence up to 30–60% of the variation in the relative abundance of Christensenellaceae across individuals.
Gut disruptors you CAN control:
Poor oral hygiene

Research in this area is still in its early days, but it’s thought that oral bacteria can travel to your gut and change your microbiome. Studies in both animals and people have indicated that oral bacteria may even alter our gut’s immune defence.
How?
Members of the oral and oropharyngeal microbiomes get to the stomach through swallowed saliva, nutrients, and drinks. Generally, these oral bacteria are poor colonisers of the healthy intestine but if they can survive the harsh acidic environment of the stomach, they may live and multiply in the gastrointestinal tract. This is especially applicable to the acid-resistant oral microbe Porphyromonas gingivalis (P.gingivalis). One animal study found that orally taken P. gingivalis changed the gut microbiome, seeing an increase in endotoxins (toxins released from certain types of bacteria), inflammatory markers and impaired gut barrier function.
Another animal study discovered that the administration of P. gingivalis considerably altered gut microbiome, with an increased proportion of the bacterial family Bacteroidetes, a decreased proportion of bacterial family Firmicutes, and increased serum endotoxin levels.
Although both generally beneficial, the Firmicutes/Bacteroidetes (F/B) ratio, made up of two of the most dominant and importantly regarded types of bacteria in the gut microbiome, is widely accepted to have an important influence in maintaining normal intestinal stability. Increased or decreased F/B ratio is regarded as dysbiosis, with the increased ratio usually observed with obesity, and the decreased ratio often seen with inflammatory bowel disease (IBD).
In the next section we talk about how different dietary habits can disrupt your gut. It’s important to remember that when you feed yourself, you’re also feeding your gut bugs. Microbes ferment prebiotics mostly found in dietary fibre and produce postbiotics as a result. Postbiotics include beneficial short chain fatty acids (SCFAs).
Highly refined carbohydrates and processed foods often seen in the Western Diet

A growing body of evidence suggests that recent lifestyle innovations, most notably the high-fat/high-sugar “Western” diet, have altered the genetic composition and metabolic activity of our gut microbes. Such diet-induced changes to gut-associated microbial communities are now suspected of contributing to growing epidemics of chronic illness in the developed world, including obesity and IBD.
Researchers have discovered that the environment created in the gut by ultra-processed foods (usually seen in a Western diet) favours microbes that can promote diverse forms of inflammatory disease. For example, a study confirmed that participants that ate a lot of fast food and savoury snacks had more Blautia, Lachnospiraceae bacteria and Clostridium bolteae in their microbiomes.
Whilst some are beneficial and produce short chain fatty acids (SCFAs), other types of Lachnospiraceae are associated with intra- and extraintestinal diseases. Clostridium bolteae is a part of a set of pathogens regularly detected in the stool samples of people affected by gastrointestinal (GI) conditions and autism symptoms. What’s more, although further studies are needed, high consumption of ultra-processed foods in men and certain subgroups of ultra-processed foods in men and women was associated with an increased risk of colorectal cancer.
How?
Gut bacteria alter their metabolism depending on the substances produced by other microbes and the nutrient supply, which may produce effects that influence metabolic and inflammatory pathways in the human body. Potentially pathological organisms which, under normal circumstances, live in harmony with the host, can cause or promote disease when specific genetic or environmental conditions are altered. This can happen with high sugar, processed foods.
For example, eating a lot of high-carbohydrate food (HCF) food like glucose, sucrose, pastas, potatoes and white bread, has been associated with significant changes in the F/B ratio in the gut bacteria.
Low dietary fibre

Microbes need to eat to survive, and they love dietary fibre! In fact, your small intestine can’t digest dietary fibre, so it passes into your colon where your gut microbes feast, breaking it down. Plant fibre and the nutrients in fruit and vegetables are favourably associated with gut bacterial diversity, which is a sign of a healthy gut. Therefore, a diet low in these foods increases the chances of an unhappy, unbalanced gut microbiome.
How?
If your gut microbes have too little dietary fibre to act upon and metabolise, not only does this hamper their survival, but also means reduction in production of short chain fatty acids (SCFAs). A review of the studies exploring the impact of dietary fibre on the gut microbiome and metabolic regulation found that dietary fibre intake increased the abundance of SCFA-producing bacteria in the gut such as Lachnospira, Akkermannsia, Bifidobacterium, Lactobacillus, Ruminococcus, Roseburia, Clostridium, Faecalibacterium, and Dorea. It also noted that previous studies indicate that certain types of soluble fibres, including inulin, beta-glucan, and GOS (galacto-oligosaccharide), may increase the abundance of SCFA-producing strains.
SCFAs are enormously beneficial to gut health and overall health. Those that result from microbial fermentation of dietary fibre have been linked to beneficial effects on host metabolic regulation. They also provide fuel for the cells lining your intestines, which act like bouncers, controlling what comes in and out as well as exerting anti-inflammatory effects.
Environmental chemical exposure

Exposure to environmental chemicals has been shown to cause changes in the gut microbiome. These disrupting chemicals that we may be exposed to frequently include:
- Bisphenols
- Phthalates
- Persistent organic pollutants
- Heavy metals
- Pesticides
How?
Bisphenol A (BPA):

Bisphenol A (BPA) is a type of plastic often used in containers that store food and beverages, such as water bottles. Animal studies have shown, amongst other things, that exposure to it increased the level of Methanobrevibacter, a type of single-celled microorganism in your gut, that can encourage you to eat more and therefore gain weight.
In mice and rabbits, exposure to BPA while they were still developing also reduced the diversity of gut microbiota composition with a decrease in protective bacteria, such as short chain fatty acid (SCFA) producers.
Phthalates:

Vinyl flooring, clothing, detergents, personal care products, children’s toys, and plastic packaging film are all sources of phthalates as are food and drinks. As well as ingesting, you can be exposed to phthalates by inhaling them as they’re also found in the environment as phthalate vapors or dust particles, absorbing it through your skin (known as dermal absorption), or through your veins, with it being found on medical equipment.
Phthalate-induced gut microbial changes in early life may change immune responses to vaccines.
Persistent organic pollutants:

Persistent organic pollutants (POPs) are poisonous chemical substances that rarely occur naturally. Rather, they’re synthesised for agricultural and industrial purposes, for instance pesticides/insecticides, fast-food packaging, non-stick coatings for cookware, and heat exchange fluids.
A human in-vitro study (one done outside of a living organism like in a test tube) found that the metabolites (intermediate or end products of metabolism) that resulted from POP-induced pollutant disturbances in the microbiome may promote the establishment of a pro-inflammatory state in the gut, illustrated by signs of the signalling protein cytokine IL-8.
Heavy metals:

Heavy metals like mercury, lead, cadmium and arsenic impact the gut microbiome. Mercury, for example, can build up in the bodies of fish in the form of methylmercury, which is highly toxic. Overall, larger and longer-lived fish tend to contain the most mercury, such as shark, swordfish, fresh tuna, marlin and king mackerel, whilst the smaller fish, such as salmon, shrimp, cod, anchovies, herring and sardines tend to be lower. Many of the smaller fish are also high in Omega-3 fatty acids which bring a whole host of benefits.
Animal studies have highlighted that arsenic alters the gut microbiome’s ability to metabolise carbohydrates and has a negative impact on the number of bacterial species that are involved in the conversion of protein to the beneficial SCFA butyrate. Other metals have differing harmful effects for example, chronic cadmium exposure resulted in significant intestinal damage and gut microbiome changes.
Pesticides:

The term ‘pesticides’ encompasses insecticides, herbicides, and fungicides and they’re generally highly toxic to target species (the pests they’re supposed to kill on plants) but we’re now learning that those pesticides that have not been banned are likely to be harmful to humans, particularly children and those exposed to pesticides through their jobs, as they can cause endocrine disruption. Your endocrine system is like a messenger network of glands that release hormones. Many pesticides, known as “legacy pesticides”, have been banned in the United States, due to their harmful effects, but their replacements have also been found to have damaging affects to non-target organs like the gut.
Most studies carried out have been on animals. For instance, Liang et al. found the pesticide Chlorpyrifos (I) caused an increased permeability of the gut lining (known as increased intestinal permeability or “leaky gut”), resulting in inflammation. Glyphosate, an herbicide found in weedkiller, was found to be toxic to the gut microbiome in an in-vitro study. The research also discovered a reduction of beneficial bacteria in the gastrointestinal tract microbiota due to glyphosate ingestion. They found this reduction could disturb the normal gut bacterial community. PAN UK have been carrying out valuable work in this area.
Pesticide residues can be found in a great variety of everyday foods and drinks, including cooked meals, water, wine, fruit juices, refreshments, and animal feeds. Exposure can occur through contact with the skin, ingestion, or inhalation, with children being even more vulnerable to exposure than adults. Although these residues in isolation may be within official safety levels, repetitive exposure over time via the sources listed above may be harmful for the body.
A note about environmental chemical exposure and our health
It’s worth noting that these chemicals can affect other aspects of our health beyond our gut:
- Bisphenol A exposure may be linked with fertility issues, a sub-optimal immune function, type-2 diabetes, and cardiovascular disease.
- Similarly, Phthalates have been associated with adverse reproductive outcomes in both women and men, for instance, type II diabetes and insulin resistance, overweight/obesity, allergy, asthma.
- Increasing evidence links POPs to reproductive disorders, neurobehavioral impairments, and immune dysfunction.
- Examples of complications of heavy metals toxic effects include kidney dysfunction, nervous system disorders, skin lesions, vascular damage, immune system dysfunction, birth defects, and cancer.
- Meanwhile, the negative health effects that have been associated with chemical pesticides include, among others, dermatological, neurological, carcinogenic, respiratory, reproductive impacts.
These health implications may not be brought about through their impact on the gut microbiome alone.
Excess alcohol consumption

Despite data being limited, research emphasises the importance of changes in the intestinal microbiota in alcohol-related disorders. Findings in a review suggest alcohol-related disorders are associated with imbalances in the intestinal microbiota and may be linked with health conditions, such as increased gastrointestinal inflammation, intestinal hyperpermeability resulting in endotoxemia (where endotoxins are present in the bloodstream), systemic inflammation throughout the body, and tissue damage/organ pathologies including alcoholic-liver disease.
How?
Alcohol-induced reduction of Bifidobacteria and higher endotoxin production has been suggested to increase intestinal inflammation in patients with gastrointestinal cancers and liver disease. Alcohol intake and the consumption of spirits have also been associated with pro-inflammatory pathways.
Disruption to the gut microbiome can happen when there’s an overall overgrowth of bacteria. Studies show that alcohol encourages both dysbiosis and bacterial overgrowth, which results in a rise in the release of endotoxins.
Artificial sweeteners and additives

Artificial sweeteners are synthetics often used as an alternative to sugar. Research is still emerging that points to artificial sweeteners and food additives, such as emulsifiers, having been found to have negative effects on the health of the gut microbiome.
In animal studies, sweeteners sucralose, aspartame, and saccharin have been shown to disrupt the balance and diversity of gut microbiome, as have two commonly used emulsifiers—carboxymethylcellulose and polysorbate-80.
Emulsifiers are added into many processed foods to improve texture and stability. They’ve been shown to shift the gut microbe population and increase low grade inflammation, heightening the risk of colon cancer in mice. However, the relevance to humans remains uncertain.
How do artificial sweeteners affect gut bacteria?

Mice given the sweetener sucralose for six months had a rise in the expression of bacterial pro-inflammatory genes in their guts and disrupted faecal metabolites. This implies that six-month sucralose consumption at the human acceptable daily intake level may increase the risk of developing tissue inflammation by disrupting the gut microbiome.
In another animal study, Splenda, which is made up of the high-potency artificial sweetener sucralose and the fillers maltodextrin and glucose, had adverse effects on male rats after 12 weeks. These effects included a drop in beneficial gut bacteria, increased faecal pH, and improved expression levels of P-gp, CYP3A4, and CYP2D1, which are known to limit the effects of orally administered drugs.
Aspartame consumption is widespread. The sweetener sold under the brand name Equal, and NutraSweet is included in more than 6000 products, including soft drinks, dessert mixes, frozen desserts and yoghurt, chewable multivitamins, and breakfast cereals and featured in about 600 pharmaceutical products.
Aspartame may influence gut metabolism and affect the gut microbiome, inducing inflammatory processes that are associated with metabolic disorders, although emerging research points to the fact that they may influence gut microbes, for certain people, more than others, depending on what their gut microbiome was to start with.
Another impact it may have is on free radicals, which you may have heard of before. One of those free radicals, reactive oxygen species (ROS) our body produces naturally, for example, as part of our energy production. However, if we have too much ROS or any other free radical this can create a state of oxidative stress – that is, an imbalance in the amount of free radicals you have in relation to antioxidants in your body which can result in damage. Consumption of aspartame can lead to excess production of the free radicals ROS and reactive nitrogen species, inducing oxidative stress and ultimately lead to inflammation and disruption to your microbiome.
Although sweeteners are used as a substitute for sugar, and one might think they’re taking the healthy option, reported side effects of certain types of sweeteners, in some individuals, especially in those who consume too much or include it in their diet for a long period of time, have included: nausea, diarrhoea and aggravation of irritable bowel syndrome and other gastrointestinal conditions.
How do emulsifiers affect gut bacteria?

In the case of emulsifiers, it was found that microbial diversity was reduced when mice were given relatively low concentrations of two common types of emulsifiers, carboxymethylcellulose (often found in milk, ice cream, baked goods and meat products) and polysorbate-80 (sources of which include commercially produced frozen desserts, baking mixes and icings, and canned vegetables) compared to mice not fed emulsifiers. This was because they had decreased amounts of the Bacteroidales and Verrucomicrobia bacteria, whilst the inflammation promoting Proteobacteria was enriched.
One of the main ways the intestine is shielded from the gut microbiome is by multi-layered mucus structures that cover its surface, allowing most gut bacteria to be kept at a safe distance from cells that line the organ. Therefore, agents that may disrupt mucus-bacterial interactions, like emulsifiers that have been seen to increase Proteobacteria, which disturb the mucosal barrier (the inner lining of the colon and rectum) and increase intestinal permeability, have the potential to promote diseases linked with gut inflammation like IBD.
Medication, especially antibiotics, PPIs and NSAIDs

Antibiotics are a common medication used to treat or prevent some bacterial infections by killing the bacteria or stopping them from spreading. It’s also not uncommon to take NSAIDs (non-steroidal anti-inflammatory drugs like ibuprofen) which, whether in tablet, capsule, cream, gel or injection form, are used to help alleviate pain, reduce inflammation, and bring down a high temperature. PPIs (proton pump inhibitors) are another form of medication that reduce the amount of acid produced by your stomach, often prescribed for acid reflux and gut and stomach ulcers. You come into contact with antibiotics, not just when prescribed by your doctor but also through their use in farm animals and crops.
Your gut microbiome is altered by exposure to antibiotics, leading to a drop in bacterial diversity. Research suggests that antibiotic exposure may lead to changes that promote long term disease and foster bacterial resistance.
If you’re prescribed an antibiotic, please ask the prescriber whether they are really necessary. If they are, ask whether you can wait to see whether the problem disappears before taking them. If that is not advised, take the antibiotic.
How do antibiotics affect the gut microbiome?
Antibiotic exposure can impact the gut microbiome in several ways, including causing the accumulation of antibiotic resistant bacteria in the gut leading to bacterial infections being untreatable by antibiotics. Repeated exposure may also result in altered insulin sensitivity and altered metabolism of short chain fatty acids (SCFA)s and bile acids – a knock on effect of this is a dis-regulated metabolism contributing to obesity, metabolic syndrome, and diabetes.
Antibiotic exposure can also see an increase in the susceptibility of intestinal infections, which can stem from newly gained pathogens or from the sudden overgrowth or pathogenic behaviour of opportunistic microbes already present in your gut microbiome.
There appears to be a link between antibiotics early in life and inflammatory and autoimmune diseases, such as allergies, asthma, IBD and irritable bowel syndrome (IBS) too, but whether the microbiome is a pathway for this is unclear.
How do PPIs affect the gut microbiome?
On a population level, the impact of PPI use on the gut microbiome is more prominent than the effects of antibiotics or other commonly used drugs. PPI use is linked to decreased bacterial richness, with 20% of the identified bacteria in a study showing significant deviation.
Bacteria that can be harmful, such as Enterococcus, Streptococcus, Staphylococcus, increased in the guts of people who used PPIs. Oral bacteria and potential pathogenic bacteria, such as Escherichia coli also increased considerably in the gut microbiome of PPI users, prompting researchers in the study to conclude that the differences between PPI users and non-users observed in their study were consistently associated with changes towards a less healthy gut microbiome.
How do NSAIDs affect the gut microbiome?
Bacteria are often classified into two broad categories: gram-negative and gram-positive. In an animal study, taking NSAIDs was shown to increase the proportion of gram-negative organisms at the expense of gram-positive organisms in the gut microbiome. This change can contribute to NSAID-induced intestinal injury. In particular, NSAIDs can decrease various members of the gram-positive bacterial class Clostridia and increase members of the gram-negative class Bacteroidia, as shown in animal studies. This may be due to the direct impact of lipopolysaccharachide (LPS) – bacterial toxins found in the outer membrane of gram-negative cell walls – and the body’s natural immune response to LPS.
Stress

Your brain and gut are constantly involved in a two-way dialogue sending signals through your gut–brain axis. When your gut receives distress signals, the increased inflammation that frequently accompanies stress triggers pathogenic bacteria in your gut that encourage dysbiosis.
How does stress affect the gut microbiome?
Stress can not only reshape the composition of your gut microbiome but can also increase the permeability of your gut lining (“leaky gut”). This means things that shouldn’t get through into your bloodstream like toxins and large food particles can suddenly get through, sparking an inflammatory response which causes further disruption to the microbiome.
It’s worth noting that the situation is complex, and it may be that the causation works in a different direction too. For instance, stress may change eating habits and increase cortisol (stress hormone) levels, which then change the microbiome and increase the permeability of the gut wall leading to more chemicals entering the blood.
Constipation

It’s still questionable whether alterations in gut microbiota are a cause or a consequence of constipation. Some studies have revealed dysbiosis of the gut microbial community may play a role in constipation.
How might gut microbiome contribute to constipation?
When it comes to studies on people with IBS with constipation, again there’s no clear consensus but research suggests that, in comparison to healthy participants, those living with the conditions had a lower level of Actinobacteria, including Bifidobacteria in their stool samples and an increased level of Bacteroidetes in their mucosa. Increases in Bacteroidetes in the colonic mucosa has also been seen in other studies.
Though more research is needed, it’s been suggested that the metabolites produced by intestinal bacteria may suppress intestinal motility, (the ability of food to move through your intestines during digestion).
How might constipation disrupt the gut microbiome?
Although there’s evidence indicating that gut dysbiosis causes constipation and IBS with constipation, can the same be said for the reverse? The answer is maybe.
The prolonged amount of time stools and waste remain in people with chronic constipation may lead to intestinal dysbiosis, which may impact the intestinal immune function, motility, and barrier function further. An animal study found that constipation in mice showed gut microbiota dysbiosis, colon inflammation and injury, and increased permeability of the intestinal barrier. It also uncovered that constipation-induced microbiota dysbiosis can lead to the increased intestinal permeability in mice.
The make-up of your gut microbiome is totally unique to you. That means that what disrupts your gut may not disrupt your friend’s gut and what supports your gut health may not necessarily have a significant impact on your family’s gut. In fact, the most accurate way to learn how to boost your individual gut health is to carry out a comprehensive stool analysis via a nutritional therapist or functional medicine doctor. That being said, below are eight wholesome habits that will improve most people’s gut health, which you can read more about here.
Reviewed by:
Anna Keeble MA BA Wellbeing Expert
Dr Brian Fisher MBBch MBE MSc FRSA – Clinical Director
- Aagaard K, Ma J, Antony KM, et al. (2014) The placenta harbors a unique microbiome. Sci Transl Med. 6: 237ra65. (doi: 10.1126/scitranslmed.300859).
- Abou-Donia MB, El-Masry EM, Abdel-Rahman AA, et al. (2008) Splenda Alters Gut Microflora and Increases Intestinal P-Glycoprotein and Cytochrome P-450 in Male Rats. Journal of Toxicology and Environmental Health, Part A 71, 2008: 1415-1429. (doi: 10.1080/15287390802328630).
- Alemao CA, Budden KF, Gomez HM, et al. (2020) Impact of diet and the bacterial microbiome on the mucous barrier and immune disorders. European Journal of Allergy and Clinical Immunology 76: Pages 714-734(doi: 10.1111/all.14548).
- Algert CS, McElduff A, Morris JM, et al. (2009) Perinatal risk factors for early onset of Type 1 diabetes in a 2000-2005 birth cohort. Diabet Med. 26: 1193-7 (doi: 10.1111/j.1464-5491.2009.02878.x.).
- André P, Laugerette F and Féart C (2019) Metabolic Endotoxemia: A Potential Underlying Mechanism of the Relationship between Dietary Fat Intake and Risk for Cognitive Impairments in Humans? Nutrients 11: 1887 (doi: 10.3390/nu11081887).
- Association for the Advancement of Restorative Medicine (n.d.) Polysorbate 80.
- Balali-Mood M, Naseri K, Tahergorabi Z, et al. (2021) Toxic Mechanisms of Five Heavy Metals: Mercury, Lead, Chromium, Cadmium, and Arsenic. Frontiers in Pharmacology (doi: 10.3389/fphar.2021.643972).
- BeMiller JN (2019) 8 – Cellulose and Cellulose-Based Hydrocolloids. Carbohydrate Chemistry for Food Scientists (Third Edition): 223-240 (doi: 10.1016/B978-0-12-812069-9.00008-X).
- Bernardi JR, Pinheiro TV, Mueller NT, et al. (2015) Cesarean delivery and metabolic risk factors in young adults: a Brazilian birth cohort study. Am J Clin Nutr. 102: 295-301 (doi: 10.3945/ajcn.114.105205).
- Bian X, Chi Liang, Gao B, et al. (2017) Gut Microbiome Response to Sucralose and Its Potential Role in Inducing Liver Inflammation in Mice. Front. Physiol. 8: 487 (doi: 10.3389/fphys.2017.00487).
- Bishehsari F, Magno E, Swanson G, et al. (2017) Alcohol and Gut-Derived Inflammation. Alcohol Res. 38: 163-171.
- Blacker RW, De Plamer G, Manko A, et al. (2015) Deciphering the pathogenesis of NSAID enteropathy using proton pump inhibitors and a hydrogen sulfide-releasing NSAID. American Journal of Physiology Gastrointestinal and Liver Physiology 308: G994-G1003. (doi: 10.1152/ajpgi.00066.2015).
- Bolte LA, Vila AV, Imhann F, et al. (2021) Long-term dietary patterns are associated with pro-inflammatory and anti-inflammatory features of the gut microbiome. Gut 70: 1287-1298 (doi: 10.1136/gutjnl-2020-322670).
- Brink LR, Mercer KR, Piccollo BD, et al. (2020) Neonatal diet alters fecal microbiota and metabolome profiles at different ages in infants fed breast milk or formula. The American Journal of Clinical Nutrition 111: 1190–1202 (doi: https://doi.org/10.1093/ajcn/nqaa076).
- Cao H, Liu X, An Y, et al. (2017) Dysbiosis contributes to chronic constipation development via regulation of serotonin transporter in the intestine. Scientific Reports 7: 10322 (doi: 10.1038/s41598-017-10835-8).
- Chassaing B, Koren O, Goodrich JK, et al. (2015) Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature 519: 92–96. (doi: 10.1038/nature14232).
- Chassard C, Dapoigny M, Scott KP, et al. (2012) Functional dysbiosis within the gut microbiota of patients with constipated-irritable bowel syndrome. Alimentary Pharmocology and Theraputics 35: 828-838 (doi: 10.1111/j.1365-2036.2012.05007.x).
- Chi L, Bian X, Goa B, et al. (2017) The Effects of an Environmentally Relevant Level of Arsenic on the Gut Microbiome and Its Functional Metagenome. Toxicological Sciences 160: 193–204 (doi: 10.1093/toxsci/kfx174).
- Chiu K, Warner G, Nowak RA, et al. (2020) The Impact of Environmental Chemicals on the Gut Microbiome. Toxicological Sciences 176: 253–284 (doi: 10.1093/toxsci/kfaa065).
- Choudhary AK and Pretorius E (2017) Revisiting the safety of aspartame. Nutrition Reviews 75: 718–730 (doi: 10.1093/nutrit/nux035).
- David LA, Maurice CF, Carmody RN, et al. (2014) Diet rapidly and reproducibly alters the human gut microbiome. Nature 505: 559–563 (doi:10.1038/nature12820).
- Decker E, Engelmann G, Findeisen A, et al. (2010) Cesarean Delivery Is Associated With Celiac Disease but Not Inflammatory Bowel Disease in Children. Pediatrics 125: e1433–e1440 (doi: 10.1542/peds.2009-2260).
- Defois C, Ratel J, Garrait G, et al. (2018) Food Chemicals Disrupt Human Gut Microbiota Activity And Impact Intestinal Homeostasis As Revealed By In Vitro Systems. Scientific Reports 8: 11006 (doi: 10.1038/s41598-018-29376-9).
- Deng F, Li Y and Zhao J (2019) The gut microbiome of healthy long-living people. Aging (Albany NY) 11: 289-290 (doi: 10.18632/aging.101771).
- Dominguez-Bello MG, Costello EK, Contreras M, et al. (2010) Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A. 107: 11971-5. (doi: 10.1073/pnas.1002601107).
- Dominguez-Bello MG, De Jesus-Laboy KM, Shen N, et al. (2016) Partial restoration of the microbiota of cesarean-born infants via vaginal microbial transfer. Nat Med. 22: 250-3 (doi: 10.1038/nm.4039).
- Dunn AB, Jordan S, Baker BJ, et al. (2017) The Maternal Infant Microbiome: Considerations for Labor and Birth. MCN Am J Matern Child Nurs. 42: 318-325 (doi: 10.1097/NMC.0000000000000373).
- Engen PA, Green SJ, Voigt RM, et al. (2015) The Gastrointestinal Microbiome: Alcohol Effects on the Composition of Intestinal Microbiota. Alcohol Res. 37: 223-36.
- Fehr K, Moossavi S, Sbihi H, et al. (2020) Breastmilk Feeding Practices Are Associated with the Co-Occurrence of Bacteria in Mothers’ Milk and the Infant Gut: the CHILD Cohort Study. Cell & Host Microbiome 28: 285-297.e4 (doi: 10.1016/j.chom.2020.06.009).
- Francino MP (2016) Antibiotics and the Human Gut Microbiome: Dysbioses and Accumulation of Resistances. Frontiers in Microbiology 6: 1543 (doi: 10.3389/fmicb.2015.01543).
- Frankenfeld CL, Hullar MAJ, Maskarinec G, et al. (2021) The Gut Microbiome Is Associated with Circulating Dietary Biomarkers of Fruit and Vegetable Intake in a Multiethnic Cohort. Journal of the Academy of Nutrition and Dietetics 122: 78-98 (doi: 10.1016/j.jand.2021.05.023).
- Goedert JJ, Hua X, Yu G, et al. (2014) Diversity and Composition of the Adult fecal Microbiome Associated with History Cesarean Birth or Appendectomy: Analysis of the American Gut Project. EBioMedicine 1: 167-172. (doi: 10.1016/j.ebiom.2014.11.004).
- Gokulan K, Arnold MG, Jensen J, et al. (2018) Exposure to Arsenite in CD-1 Mice during Juvenile and Adult Stages: Effects on Intestinal Microbiota and Gut-Associated Immune Status. mBio 9 (doi: 10.1128/mBio.01418-18).
- Goodrich JK, Waters JL, Poole AC, et al. (2014) Human Genetics Shape the Gut Microbiome. Cell 159: P789-799 (doi: 10.1016/j.cell.2014.09.053).
- Grölund, M-M, Lehtonen, OP†; Eerola, E,et al. (1999) Fecal Microflora in Healthy Infants Born by Different Methods of Delivery: Permanent Changes in Intestinal Flora After Cesarean Delivery. Journal of Pediatric Gastroenterology & Nutrition 28: 19-25.
- Guo C, Zhou Q, Li M, et al. (2020) Breastfeeding restored the gut microbiota in caesarean section infants and lowered the infection risk in early life. BMC Pediatrics 20: 532.
- Hagiwara M, Kataoka K, Arimochi H, et al. (2004) Role of unbalanced growth of Gram-negetive bacteria in ilealulcer formation in rats treated with a nonsteroidal anti-inflammatory drug. Journal of Medical Investigation 51: 43-51 (doi: 10.2152/jmi.51.43).
- Huërou-Luron IL, Blat S and Boudry G (2010) Breast- v. formula-feeding: impacts on the digestive tract and immediate and long-term health effects. Nutrition Research Reviews 23: 23-36 (doi: 10.1017/S0954422410000065).
- Imhann F, Bonder MJ, Vila AV, et al. (2016) Proton pump inhibitors affect the gut microbiome. Gut 65: 740-748. (doi: 10.1136/gutjnl-2015-310376).
- Javurek AB, Spollen WG, Johnson SA, et al. (2016) Effects of exposure to bisphenol A and ethinyl estradiol on the gut microbiota of parents and their offspring in a rodent model. Gut Microbes 7: 471-485 (doi: 10.1080/19490976.2016.1234657).
- Knott L and Willacy H (2020) Proton Pump Inhibitors. Patient.
- Koh A, Vadder FD, Kovatcheva-Datchary P, et al. (2016) From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell 165: 1332-1345 (doi: 10.1016/j.cell.2016.05.041).
- Korpela K, Helve O, Kolho K-L, et al. (2020) Maternal Fecal Microbiota Transplantation in Cesarean-Born Infants Rapidly Restores Normal Gut Microbial Development: A Proof-of-Concept Study. Cell 183: 324-334.e5 (doi: 10.1016/j.cell.2020.08.047).
- Li HT, Zhou YB and Liu JM, (2013) The impact of cesarean section on offspring overweight and obesity: a systematic review and meta-analysis. International Journal of Obesity 37: 893–899 (doi: 10.1038/ijo.2012.195).
- Li QQ, Loganath A, Chong YS, et al. (2006) Persistent Organic Pollutants and Adverse Health Effects in Humans. Journal of Toxicology and Environmental Health, Part A. 69: 1987-2005 (doi: 10.1080/15287390600751447).
- Liang Y, Zhan J, Liu D, et al. (2019) Organophosphorus pesticide chlorpyrifos intake promotes obesity and insulin resistance through impacting gut and gut microbiota. Microbiome 7: 19. (doi: 10.1186/s40168-019-0635-4).
- Lin X, Liu Y, Ma L, et al. (2021) Constipation induced gut microbiota dysbiosis exacerbates experimental autoimmune encephalomyelitis in C57BL/6 mice. J Transl Med. 19: 317 (doi: 10.1186/s12967-021-02995-z).
- Ma J, Li Z, Zhang W, et al. (2020) Comparison of gut microbiota in exclusively breast-fed and formula-fed babies: a study of 91 term infants. Scientific Reports 15792 (doi: 10.1038/s41598-020-72635-x).
- Mackie RI, Sghir A, Gaskins HR (1999) Developmental microbial ecology of the neonatal gastrointestinal tract. The American Journal of Clinical Nutrition 69: 1035s–1045s (doi: 10.1093/ajcn/69.5.1035s).
- Madison A and Kiecolt-Glaser JK (2019) Stress, depression, diet, and the gut microbiota: human-bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr Opin Behav Sci. 28: 105-110 (doi: 10.1016/j.cobeha.2019.01.011).
- Messer JS and Chang EB (2018) Chapter 36 – Microbial Physiology of the Digestive Tract and Its Role in Inflammatory Bowel Diseases. Physiology of the Gastrointestinal Tract (Sixth Edition): 795-810 (doi: 10.1016/B978-0-12-809954-4.00036-0).
- Mnif W, Hassine AIH, Bouaziz A, et al. (2011) Effect of Endocrine Disruptor Pesticides: A Review. Int. J. Environ. Res. Public Health 8: 2265-2303 (doi: 10.3390/ijerph8062265).
- Moossavi S and Azad MB (2019) Origins of human milk microbiota: new evidence and arising questions. Gut Microbes 12 (doi: 10.1080/19490976.2019.1667722).
- Mueller NT, Bakacs E, Combellick J, et al. (2014) The infant microbiome development: mom matters. Trends Mol Med. 21: 109-17 (doi: 10.1016/j.molmed.2014.12.002).
- Mutlu EA, Gillevet PM, Rangwala H, et al. (2012) Colonic microbiome is altered in alcoholism. American Journal of Physiology-Gastrointestinal and Liver Physiology 302: G966-G978 (doi: 10.1152/ajpgi.00380.2011).
- Myhrstad MCW, Tunsjø H, Charnock C, et al. (2020) Dietary Fiber, Gut Microbiota, and Metabolic Regulation-Current Status in Human Randomized Trials. Nutrients 12: 859 (doi: 10.3390/nu12030859).
- Nakajima M, Arimatsu K, Kato T, et al. (2015) Oral Administration of P. gingivalis Induces Dysbiosis of Gut Microbiota and Impaired Barrier Function Leading to Dissemination of Enterobacteria to the Liver. PLoS ONE 10: e0134234. (doi: 10.1371/journal.pone.0134234).
- NHS (2019) NSAIDs.
- NHS (2019) Overview-Antibiotics.
- Nicolopoulou-Stamati P, Maipas S, Kotampasi C, et al. (2016) Chemical Pesticides and Human Health: The Urgent Need for a New Concept in Agriculture. Front Public Health. 4:148. (doi: 10.3389/fpubh.2016.00148).
- Nogal A, Valdes AM and Menni C (2021) The role of short-chain fatty acids in the interplay between gut microbiota and diet in cardio-metabolic health. Gut Microbes 13 (doi: 10.1080/19490976.2021.1897212).
- Ohkusa T, Koido S, Nishikawa Y, et al. (2019) Gut Microbiota and Chronic Constipation: A Review and Update. Front Med (Lausanne) 6:19 (doi: 10.3389/fmed.2019.00019).
- Olsen I and Yamazaki K (2019) Can oral bacteria affect the microbiome of the gut? J Oral Microbiol. 11: 1586422 (doi: 10.1080/20002297.2019.1586422).
- Pannaraj PS, Li F, Cerini C, et al. (2017) Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 171: 647-654. (doi: 10.1001/jamapediatrics.2017.0378).
- Parkes GC, Rayment NB, Hudspith BN, et al. (2011) Distinct microbial populations exist in the mucosa-associated microbiota of sub-groups of irritable bowel syndrome. Neurogastoenterology & Motility 24: 31-39 (doi: 10.1111/j.1365-2982.2011.01803.x).
- Parthasarathy G, Chen J, Chen X, et al. (2015) Relationship Between Microbiota of the Colonic Mucosa vs Feces and Symptoms, Colonic Transit, and Methane Production in Female Patients With Chronic Constipation. Clinical – Aolimentary Tract 150: 367-379 (doi: 10.1053/j.gastro.2015.10.005).
- Pepino MY and Bourne C (2011) Non-nutritive sweeteners, energy balance, and glucose homosatis. Current Opinion in Clinical Nutrition and Metabolic Care 14: 391-395 (doi: 10.1097/MCO.0b013e3283468e7e).
- Pequegnat B and Monteiro MA (2019) Carbohydrate Scaffolds for the Study of the Autism-associated Bacterium, Clostridium bolteae. Curr Med Chem. 26: 6341–6348. (doi: 10.2174/0929867326666190225164527).
- Pesticide Action Network UK (n.d.) Glypohsate.
- Pesticide Action Network UK (n.d.) Impacts of pesticides on our health.
- Rao RK, Seth A and Sheth P (2004) Recent Advances in Alcoholic Liver Disease I. Role of intestinal permeability and endotoxemia in alcoholic liver disease. American Journal of Physiology-Gastrointestinal and Liver Physiology 286: G881-G884 (doi: 10.1152/ajpgi.00006.2004).
- Reddivari L, Veeramachaneni DNR, Walters WA, et al. (2017) Perinatal Bisphenol A Exposure Induces Chronic Inflammation in Rabbit Offspring via Modulation of Gut Bacteria and Their Metabolites. ASM Journals mSystems 2 (doi: 10.1128/mSystems.00093-17).
- Rizzatti G, Lopetuso LR, Gibiino G, et al. (2017) Proteobacteria: A Common Factor in Human Diseases. BioMed Research International 2017: 9351507 (doi: 10.1155/2017/9351507).
- Roberts JR, Karr CJ, Council On Environmental Health (2012) Pesticide exposure in children. Pediatrics 130: e1765-88 (doi: 10.1542/peds.2012-2758).
- Rochester JR (2013) Bisphenol A and human health: A review of the literature. Reproductive Toxicology 42: 132-155 (doi: 10.1016/j.reprotox.2013.08.008).
- Salminen S, Gibson GR, McCartney AL, et al. (2004) Influence of mode of delivery on gut microbiota composition in seven year old children. Gut. 53: 1388-9 (doi: 10.1136/gut.2004.041640).
- Sato K, Takahashi N, Kato T, et al. (2017) Aggravation of collagen-induced arthritis by orally administered Porphyromonas gingivalis through modulation of the gut microbiota and gut immune system. Scientific Reports 7: 6955 (doi: 10.1038/s41598-017-07196-7).
- Schnabl B and Brenner DA (2014) Interactions Between the Intestinal Microbiome and Liver Diseases. The Gut Microbiome and Disease 146: 1513-1524 (doi: 10.1053/j.gastro.2014.01.020).
- Sela DA, Chapman J, Adeuya A, et al. (2008) The genome sequence of Bifidobacterium longumsubsp.infantisreveals adaptations for milkutilization within the infant microbiome. PNAS 105: 18969.
- Shao Y, Forster SC, Tsaliki E, et al. (2019) Stunted microbiota and opportunistic pathogen colonization in caesarean-section birth. Nature 574: 117-121 (doi: 10.1038/s41586-019-1560-1).
- Shehata AA, Schrödl W, Aldin AA, et al. (2013) The Effect of Glyphosate on Potential Pathogens and Beneficial Members of Poultry Microbiota In Vitro. Current Microbiology 66: 350–358 (doi: 10.1007/s00284-012-0277-2).
- Song SE, Wang J and Martino C, et al. (2021) Naturalization of the microbiota developmental trajectory of Cesarean-born neonates after vaginal seeding. Med. 2: P951-964.E5 (doi: 10.1016/j.medj.2021.05.003).
- Storelli MM and Marcotrigiano (2010) Fish for human consumption: risk of contamination by mercury. Food additives and Contaminants 17 2000: 1007-1011. (doi: 10.1080/02652030050207792).
- Stojanov S, Berlec A and Strukelj B (2020) The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel disease. Microorganisms 8: 1715 (doi: 10.3390/microorganisms8111715).
- Stout MJ, Conlon B, Landeau M, et al. (2013) Identification of intracellular bacteria in the basal plate of the human placenta in term and preterm gestations. Am J Obstet Gynecol. 208: 226.e1-7 (doi: 10.1016/j.ajog.2013.01.018).
- Suez J, Cohen Y, Valdés-Mas R, et al. (2022) Personalized microbiome-driven effects of non-nutritive sweeteners on human glucose tolerance. Cell 185: 3307-3328 (doi: 10.1016/j.cell.2022.07.016).
- Sweeney TE and Morton TM (2013) The Human Gut Microbiome A Review of the Effect of Obesity and Surgically Induced Weight Loss. JAMA Surg. 148: 563-569 (doi:10.1001/jamasurg.2013.5).
- Togo A, Dufour J-C, Lagier J-C, et al. (2018) Repertoire of human breast and milk microbiota: a systematic review. Future Microbiology 14 (doi: 10.2217/fmb-2018-031).
- Turnbaugh PJ, Hamady M, Yatsunenko T, et al. (2009) A core gut microbiome in obese and lean twins. Nature 457: 480–484. (doi: 10.1038/nature07540).
- U.S. Food & Drug Association (2014) Mercury Levels in Commercial Fish and Shellfish (1990 – 2012).
- Vacca M, Celano G, Calabrese FM, et al. (2020) The Controversial Role of Human Gut Lachnospiraceae. Microorganisms 8: 473 (doi: 10.3390/microorganisms8040573).
- Valdes AM, Walter J, Segal E, et al. (2018) Role of the gut microbiota in nutrition and health. BMJ 361: k2179 (doi:10.1136/bmj.k2179).
- van den Elsen LWJ, Garssen J, Burcelin R, et al. (2019) Shaping the Gut Microbiota by Breastfeeding: The Gateway to Allergy Prevention? Front Pediatr. 7:47 (doi: 10.3389/fped.2019.00047).
- Venegas DP, De la Fuente MK, Landskron G, et al. (2019) Short Chain Fatty Acids (SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases. Front. Immunol.10: 277. (doi: 10.3389/fimmu.2019.00277).
- Vernocchi P, Chierico FD and Putignani L (2020) Gut Microbiota Metabolism and Interaction with Food Components. Int J Mol Sci. 21: 3688 (doi: 10.3390/ijms21103688).
- Viennois E, Merlin D, Gewirtz AT, et al. (2017) Dietary Emulsifier-Induced Low-Grade Inflammation Promotes Colon Carcinogenesis. Cancer Res. 77: 27-40 (doi: 10.1158/0008-5472.CAN-16-1359).
- Walker MY, Pratap S, Southerland JH, et al. (2018) Role of oral and gut microbiome in nitric oxide-mediated colon motility. Nitric Oxide 73: 81-88. (doi: 10.1016/j.niox.2017.06.003).
- Wang JK and Yao SK. Roles of Gut Microbiota and Metabolites in Pathogenesis of Functional Constipation. Evid Based Complement Alternat Med. 2021: 5560310 (doi: 10.1155/2021/5560310).
- Wang Y and Qian H (2021) Phthalates and Their Impacts on Human Health. Healthcare (Basel) 9: 603 (doi: 10.3390/healthcare9050603).
- Whitfield-Cargile CM, Cohen ND, Chapkin RS, et al. (2016) The microbiota-derived metabolite indole decreases mucosal inflammation and injury in murine model of NASAID Enteropathy. Gut Microbes 7: 246-271 (doi: 10.1080/19490976.2016.1156827).
- Wang L, Du M, Wang K, et al. (2022) Association of ultra processed food consumption with colorectal cancer risk among men and women: results from three prospective US cohort studies. BMJ 378: e068921 (doi: 10.1136/bmj-2021-068921).
- Wilson BC, Butler EM, Grigg CP, et al. (2021) Oral administration of maternal vaginal microbes at birth to restore gut microbiome development in infants born by caesarean section: A pilot randomised placebo-controlled trial. eBioMedicine 69, 103443 (doi: 10.1016/j.ebiom.2021.103443).
- Wittassek M, Koch HM, Angerer J, et al. (2011) Assessing exposure to phthalates – The human biomonitoring approach. Molecular Nutrition & Food Research 55: 7-31 (doi: 10.1002/mnfr.201000121).
- Ya J, Ju Z, Wang H, et al. (2019) Exposure to cadmium induced gut histopathological damages and microbiota alterations of Chinese toad (Bufo gargarizans) larvae. Ecotoxicology and Environmental Safety 180: 449-456 (doi: 10.1016/j.ecoenv.2019.05.038).
- Yang Y-N, Yang Y-C SH, Lin I-H, et al. (2019) Phthalate exposure alters gut microbiota composition and IgM vaccine response in human newborns. Food and Chemical Toxicology 132 (doi: 10.1016/j.fct.2019.110700).
- Zinöcker MK and Lindseth IA (2018) The Western Diet–Microbiome-Host Interaction and Its Role in Metabolic Disease. Nutrients 10: 365 (doi: 10.3390/nu10030365).